Sunday Poster Session
Category: Biliary/Pancreas
P0147 - A Stone Rarer Than a Diamond: A Case of Primary Choledocholithiasis 53 Years After Cholecystectomy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Michelle Livitz, DO
Louisiana State University
New Orleans, LA
Presenting Author(s)
Michelle Livitz, DO
Louisiana State University, New Orleans, LA
Introduction: Post-cholecystectomy syndrome (PCS) is a common phenomenon defined as a persistence of biliary colic or RUQ abdominal pain with associated GI symptoms following a cholecystectomy. Known etiologies include retained calculi, bile leak, biliary strictures, and dyskinesia of the sphincter of Oddi. Incidence in literature ranges from 5-30%, and of those, 26% are noted to be from functional disorders. Most common presentation is within the first 3 years post-operatively.
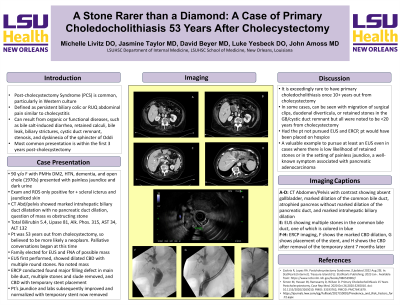
Case Description/Methods: 90 y/o F with history of DM2, HTN, dementia, and open cholecystectomy (1970s) presented for painless jaundice and dark urine. Last known normal was 2 days prior to presentation per family. Patient denied abdominal pain, changes in stool, nausea, or fevers. On exam, she was jaundiced with scleral icterus, but no abdominal distension, tenderness, or other pertinent findings. A CT abdomen with contrast showed intrahepatic biliary duct dilatation without pancreatic duct dilatation, concerning for obstructing gallstone versus ampullary mass. Labs were notable for elevated total bilirubin 5.4, lipase 81, alkaline phosphatase 315, AST 34, and ALT 132: indicative of cholestasis. Since her cholecystectomy was 53 years prior, primary concern was malignancy. Hospice was discussed given age, mental status, and worsened quality of life with further treatment. She was ultimately evaluated with EUS to perform FNA of suspected mass, followed by an ERCP. During the EUS, there was 20mm CBD dilation, multiple stones with characteristic shadowing seen, and no signs of pathology in the ampulla. Subsequent ERCP noted a filling defect in the CBD. A 15 mm balloon swept the duct for biliary sludge and stones, and a stent was placed in the distal third of the CBD at the site of a fibrotic stricture causing severe stenosis, with subsequent bile flow. Post-op labs showed improvement of the patient’s bilirubin, AP, and LFTs, and she was discharged the following day.
Discussion: It is rare for patients to present with primary choledocholithiasis once they are >10 years from their cholecystectomy. In the few case reports that have been written, it is typically secondary to migrated surgical clips or retained stones in the biliary tract. The long latency period in this patient is remarkable; but more notably, the clinical course was almost deviated toward hospice initiation for a reversible medical condition. This case is a valuable example of the importance of considering PCS, even decades later, in the setting of painless jaundice.

Disclosures:
Michelle Livitz, DO. P0147 - A Stone Rarer Than a Diamond: A Case of Primary Choledocholithiasis 53 Years After Cholecystectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Louisiana State University, New Orleans, LA
Introduction: Post-cholecystectomy syndrome (PCS) is a common phenomenon defined as a persistence of biliary colic or RUQ abdominal pain with associated GI symptoms following a cholecystectomy. Known etiologies include retained calculi, bile leak, biliary strictures, and dyskinesia of the sphincter of Oddi. Incidence in literature ranges from 5-30%, and of those, 26% are noted to be from functional disorders. Most common presentation is within the first 3 years post-operatively.
Case Description/Methods: 90 y/o F with history of DM2, HTN, dementia, and open cholecystectomy (1970s) presented for painless jaundice and dark urine. Last known normal was 2 days prior to presentation per family. Patient denied abdominal pain, changes in stool, nausea, or fevers. On exam, she was jaundiced with scleral icterus, but no abdominal distension, tenderness, or other pertinent findings. A CT abdomen with contrast showed intrahepatic biliary duct dilatation without pancreatic duct dilatation, concerning for obstructing gallstone versus ampullary mass. Labs were notable for elevated total bilirubin 5.4, lipase 81, alkaline phosphatase 315, AST 34, and ALT 132: indicative of cholestasis. Since her cholecystectomy was 53 years prior, primary concern was malignancy. Hospice was discussed given age, mental status, and worsened quality of life with further treatment. She was ultimately evaluated with EUS to perform FNA of suspected mass, followed by an ERCP. During the EUS, there was 20mm CBD dilation, multiple stones with characteristic shadowing seen, and no signs of pathology in the ampulla. Subsequent ERCP noted a filling defect in the CBD. A 15 mm balloon swept the duct for biliary sludge and stones, and a stent was placed in the distal third of the CBD at the site of a fibrotic stricture causing severe stenosis, with subsequent bile flow. Post-op labs showed improvement of the patient’s bilirubin, AP, and LFTs, and she was discharged the following day.
Discussion: It is rare for patients to present with primary choledocholithiasis once they are >10 years from their cholecystectomy. In the few case reports that have been written, it is typically secondary to migrated surgical clips or retained stones in the biliary tract. The long latency period in this patient is remarkable; but more notably, the clinical course was almost deviated toward hospice initiation for a reversible medical condition. This case is a valuable example of the importance of considering PCS, even decades later, in the setting of painless jaundice.

Figure: A. First image of Biliary tree prior to intervention
B. Final image of Biliary tree after stent placement
B. Final image of Biliary tree after stent placement
Disclosures:
Michelle Livitz indicated no relevant financial relationships.
Michelle Livitz, DO. P0147 - A Stone Rarer Than a Diamond: A Case of Primary Choledocholithiasis 53 Years After Cholecystectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
