Sunday Poster Session
Category: Biliary/Pancreas
P0149 - Right Hepatic Duct Intraductal Papillary Neoplasm of the Bile Duct: A Rare Cause of Obstructive Jaundice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DC
David L. Cheung, MD
UC Irvine
Orange, CA
Presenting Author(s)
Award: Presidential Poster Award
David L. Cheung, MD1, Andy Lin, MD2, Amirali Tavangar, MD2, Peter Nguyen, MD2, Joshua Kwon, MD2, Khaldoon Khirfan, MD2, Jason Samarasena, MD2, John Lee, MD2
1UC Irvine, Orange, CA; 2University of California Irvine, Orange, CA
Introduction: Intraductal papillary neoplasms of the bile duct (IPNB) are the rare biliary cousins to the pancreatic intraductal papillary mucinous neoplasms (IPMN). While both mucin-producing and with malignant potential, IPNBs grow within the hepatobiliary tree with a prevalence of 4-15% of bile duct tumors. Here, we present a rare case of IPNB within the right hepatic and cystic duct.
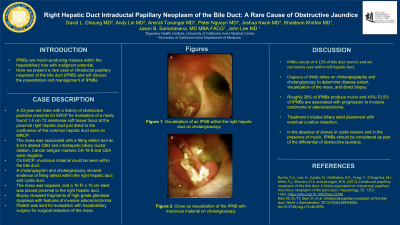
Case Description/Methods: A 53-year-old male with a history of obstructive jaundice presents for ERCP for evaluation of a newly found 1.4 cm T2 isointense soft tissue focus at the proximal right hepatic duct just distal to the confluence of the common hepatic duct seen on MRCP (Image A/B). The mass was associated with a filling defect and an 8 mm dilated CBD and intrahepatic biliary ductal dilation. Cancer antigen markers CA-19-9 and CEA were negative. On ERCP, mucinous material could be seen within the bile duct (Image B). A cholangiogram and cholangioscopy showed evidence of filling defect within the right hepatic duct and cystic duct. The mass was biopsied, and a 10 Fr x 15 cm stent was placed proximal to the right hepatic duct. The biopsy revealed fragments of high-grade glandular dysplasia with features of invasive adenocarcinoma. The patient was, subsequently, sent for evaluation with hepatobiliary surgery for surgical resection of the mass.
Discussion: Commonly seen more in Eastern Asian countries with risk factors for hepatolithiasis and chlonorchiasis and within the left intrahepatic duct, IPNB within the right hepatic duct are extremely rare. While accurate diagnosis of IPNBs is difficult as imaging may not always pick up tumors or the presence of mucin, cholangiography and cholangioscopy are mainstay diagnostic techniques to determine disease extent, visualization of the mass, and direct biopsy. Interestingly, only roughly 28% of IPNBs produce mucin and 43%-70.5% of IPNBs are associated with progression to invasive carcinoma or adenocarcinoma. Given the high-risk recurrent hepatobiliary obstruction and risk for malignancy, the mainstay treatment includes biliary stent placement with eventual curative resection. For this case, direct visualization with cholangioscopy was necessary to biopsy the lesion and make the diagnosis. In the absence of stones or cystic lesions and in the presence of mucin, IPNBs should be considered as part of the differential of obstructive jaundice.

Disclosures:
David L. Cheung, MD1, Andy Lin, MD2, Amirali Tavangar, MD2, Peter Nguyen, MD2, Joshua Kwon, MD2, Khaldoon Khirfan, MD2, Jason Samarasena, MD2, John Lee, MD2. P0149 - Right Hepatic Duct Intraductal Papillary Neoplasm of the Bile Duct: A Rare Cause of Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
David L. Cheung, MD1, Andy Lin, MD2, Amirali Tavangar, MD2, Peter Nguyen, MD2, Joshua Kwon, MD2, Khaldoon Khirfan, MD2, Jason Samarasena, MD2, John Lee, MD2
1UC Irvine, Orange, CA; 2University of California Irvine, Orange, CA
Introduction: Intraductal papillary neoplasms of the bile duct (IPNB) are the rare biliary cousins to the pancreatic intraductal papillary mucinous neoplasms (IPMN). While both mucin-producing and with malignant potential, IPNBs grow within the hepatobiliary tree with a prevalence of 4-15% of bile duct tumors. Here, we present a rare case of IPNB within the right hepatic and cystic duct.
Case Description/Methods: A 53-year-old male with a history of obstructive jaundice presents for ERCP for evaluation of a newly found 1.4 cm T2 isointense soft tissue focus at the proximal right hepatic duct just distal to the confluence of the common hepatic duct seen on MRCP (Image A/B). The mass was associated with a filling defect and an 8 mm dilated CBD and intrahepatic biliary ductal dilation. Cancer antigen markers CA-19-9 and CEA were negative. On ERCP, mucinous material could be seen within the bile duct (Image B). A cholangiogram and cholangioscopy showed evidence of filling defect within the right hepatic duct and cystic duct. The mass was biopsied, and a 10 Fr x 15 cm stent was placed proximal to the right hepatic duct. The biopsy revealed fragments of high-grade glandular dysplasia with features of invasive adenocarcinoma. The patient was, subsequently, sent for evaluation with hepatobiliary surgery for surgical resection of the mass.
Discussion: Commonly seen more in Eastern Asian countries with risk factors for hepatolithiasis and chlonorchiasis and within the left intrahepatic duct, IPNB within the right hepatic duct are extremely rare. While accurate diagnosis of IPNBs is difficult as imaging may not always pick up tumors or the presence of mucin, cholangiography and cholangioscopy are mainstay diagnostic techniques to determine disease extent, visualization of the mass, and direct biopsy. Interestingly, only roughly 28% of IPNBs produce mucin and 43%-70.5% of IPNBs are associated with progression to invasive carcinoma or adenocarcinoma. Given the high-risk recurrent hepatobiliary obstruction and risk for malignancy, the mainstay treatment includes biliary stent placement with eventual curative resection. For this case, direct visualization with cholangioscopy was necessary to biopsy the lesion and make the diagnosis. In the absence of stones or cystic lesions and in the presence of mucin, IPNBs should be considered as part of the differential of obstructive jaundice.

Figure: A) Visualization of IPNB within the right hepatic duct on cholangioscopy
B) Close up visualization of IPNB with mucinous material on cholangioscopy
B) Close up visualization of IPNB with mucinous material on cholangioscopy
Disclosures:
David Cheung indicated no relevant financial relationships.
Andy Lin indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Joshua Kwon indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Jason Samarasena: Applied Medical – Advisor or Review Panel Member. Boston Scientific – Consultant. Conmed – Consultant. Cook – Educational Grant. Neptune Medical – Consultant. Olympus – Consultant. Steris – Consultant.
John Lee indicated no relevant financial relationships.
David L. Cheung, MD1, Andy Lin, MD2, Amirali Tavangar, MD2, Peter Nguyen, MD2, Joshua Kwon, MD2, Khaldoon Khirfan, MD2, Jason Samarasena, MD2, John Lee, MD2. P0149 - Right Hepatic Duct Intraductal Papillary Neoplasm of the Bile Duct: A Rare Cause of Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


