Sunday Poster Session
Category: Biliary/Pancreas
P0156 - Recurrent Alcohol-Associated Pancreatitis Complicated by Pancreatico-Pleural Fistula: Endoscopic Management
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Amber Cloud, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Amber Cloud, MD, Kshitij Thakur, MD, MSc, Ujas Patel, MD, Samuel Mardini, MD, MBA, MPH
University of Kentucky, Lexington, KY
Introduction: Here we present a case of a young male with a pancreatico-pleural fistula, a rare complication associated with recurrent pancreatitis.
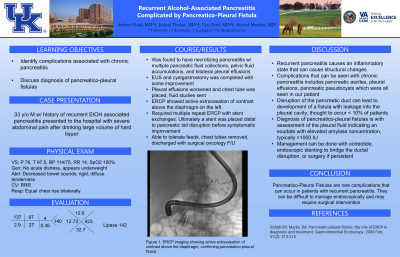
Case Description/Methods: We present the case of a 33-year-old male with recurrent alcoholic pancreatitis, who presented with severe abdominal pain after consuming a large volume of hard liquor. Evaluation revealed necrotizing pancreatitis with peripancreatic and pelvic fluid collections. Subsequently, the patient developed large left and moderate right pleural effusions, extending mediastinally from the peri-pancreatic fluid collection. Interventional radiology-guided left-sided chest tube placement and fluid studies were conducted showing a high amylase level. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a pancreatico-pleural fistula, exhibiting active contrast extravasation above the left diaphragm. A medium-sized pancreatic sphincterotomy and placement of a single pigtail plastic stent in the pancreatic duct were performed. Over the subsequent two months, the patient underwent repeated ERCPs and stent exchanges. The surgical team considered the patient a candidate for distal pancreatectomy once the acute phase of pancreatitis resolved. After two months repeat ERCP showed persistent but improved pancreatic duct disruption. Stents were exchanged, placing a new stent distal to the disruption in the pancreatic tail. Following this procedure, the patient experienced pain relief, tolerated feeds, and had his chest tubes removed. He was discharged with plans for outpatient ERCP and follow-up with surgical oncology.
Discussion: Recurrent pancreatitis can lead to permanent structural changes and various complications, including pancreatic ascites, pleural effusions, and pancreatic pseudocysts. Pancreatic duct disruption may result in the formation of a fistula, such as the pancreatico-pleural fistula observed in our patient, leading to pancreatic fluid leakage into the pleural cavity. This complication occurs in less than 10% of patients with pseudocysts. Diagnosis involves evaluating pleural fluid, which typically exhibits exudative characteristics with elevated amylase concentration ( >1000 international units). Conservative management with octreotide to decrease pancreatic secretion may be attempted but often requires endoscopic stenting to bridge the ductal disruption. If the fistula persists, surgical intervention is often necessary.

Disclosures:
Amber Cloud, MD, Kshitij Thakur, MD, MSc, Ujas Patel, MD, Samuel Mardini, MD, MBA, MPH. P0156 - Recurrent Alcohol-Associated Pancreatitis Complicated by Pancreatico-Pleural Fistula: Endoscopic Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: Here we present a case of a young male with a pancreatico-pleural fistula, a rare complication associated with recurrent pancreatitis.
Case Description/Methods: We present the case of a 33-year-old male with recurrent alcoholic pancreatitis, who presented with severe abdominal pain after consuming a large volume of hard liquor. Evaluation revealed necrotizing pancreatitis with peripancreatic and pelvic fluid collections. Subsequently, the patient developed large left and moderate right pleural effusions, extending mediastinally from the peri-pancreatic fluid collection. Interventional radiology-guided left-sided chest tube placement and fluid studies were conducted showing a high amylase level. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a pancreatico-pleural fistula, exhibiting active contrast extravasation above the left diaphragm. A medium-sized pancreatic sphincterotomy and placement of a single pigtail plastic stent in the pancreatic duct were performed. Over the subsequent two months, the patient underwent repeated ERCPs and stent exchanges. The surgical team considered the patient a candidate for distal pancreatectomy once the acute phase of pancreatitis resolved. After two months repeat ERCP showed persistent but improved pancreatic duct disruption. Stents were exchanged, placing a new stent distal to the disruption in the pancreatic tail. Following this procedure, the patient experienced pain relief, tolerated feeds, and had his chest tubes removed. He was discharged with plans for outpatient ERCP and follow-up with surgical oncology.
Discussion: Recurrent pancreatitis can lead to permanent structural changes and various complications, including pancreatic ascites, pleural effusions, and pancreatic pseudocysts. Pancreatic duct disruption may result in the formation of a fistula, such as the pancreatico-pleural fistula observed in our patient, leading to pancreatic fluid leakage into the pleural cavity. This complication occurs in less than 10% of patients with pseudocysts. Diagnosis involves evaluating pleural fluid, which typically exhibits exudative characteristics with elevated amylase concentration ( >1000 international units). Conservative management with octreotide to decrease pancreatic secretion may be attempted but often requires endoscopic stenting to bridge the ductal disruption. If the fistula persists, surgical intervention is often necessary.

Figure: Extravasation of contrast above the diaphragm
Disclosures:
Amber Cloud indicated no relevant financial relationships.
Kshitij Thakur indicated no relevant financial relationships.
Ujas Patel indicated no relevant financial relationships.
Samuel Mardini indicated no relevant financial relationships.
Amber Cloud, MD, Kshitij Thakur, MD, MSc, Ujas Patel, MD, Samuel Mardini, MD, MBA, MPH. P0156 - Recurrent Alcohol-Associated Pancreatitis Complicated by Pancreatico-Pleural Fistula: Endoscopic Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
