Sunday Poster Session
Category: Colon
P0175 - Assessing Acute Kidney Injury in Patients With Cirrhosis and Clostridium difficile Infection: A 5-Year National Inpatient Sample Analysis of Hospital Complications
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Het Patel, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Het Patel, DO1, Naomi Reddy-Patel, MD2, Zarian Prenatt, DO1, Hammad Liaquat, MD2
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Clostridium Difficile Infection (CDI) has a greater incidence in patients with liver cirrhosis for multiple reasons such as recurrent hospitalizations, immunodeficiency, and long-term antibiotic use. Cirrhosis also has profound effects on the body’s baseline hemodynamics and renin-angiogenin-aldosterone system. The aim of the study is to assess the risk of adverse outcomes of acute kidney injury (AKI) in patients with CDI and cirrhosis.
Methods: This is a retrospective cohort study using National Inpatient Sample data including adults with history of liver cirrhosis hospitalized between 2016 and 2020 presenting with CDI. The primary outcome measured was inpatient complications in patients with AKI. Statistical analyses were all performed using STATA software.
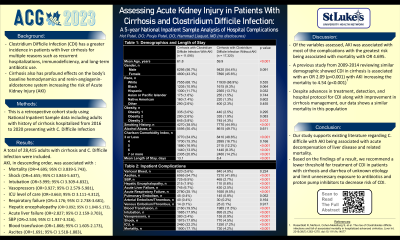
Results: Of the 28,415 patients with cirrhosis who presented with CDI, 11,095 (39%) patients had AKI of which 56.7% were males and 68.1% were Caucasian. Patients with class obesity 3, malnutrition, length of stay and Charlson Comorbidity Index (CCI) of 5 or more had statistically significant (p< 0.05) association with AKI while CCI of 3 or less and smoking history was protective (Table 1). Patients with AKI were associated with ascites (OR=1.691; 95% CI 1.518-1.883), SBP (OR=2.534; 95% CI 1.937-3.316), hepatic encephalopathy (OR=3.092; 95% CI 1.848-5.172), acute liver failure (OR=2.827; 95% CI 2.159-3.703), acute respiratory failure (OR=3.176; 95% CI 2.738-3.681), shock (OR=4.655; 95% CI 3.844-5.637), and mortality (OR=4.695; 95% CI 3.839-5.743). Patients with AKI were also associated with increased requirement of blood transfusion (OR=1.868; 95% CI 1.605-2.173), intubation (OR=3.999; 95% CI 3.309-4.832), vasopressors (OR=3.927; 95% CI 2.579-5.981), and ICU level of care (OR=3.663; 95% CI 3.111-4.312) (Table 2). Patients with PBC did not have a statistically significant association (p >0.05) with variceal bleed, arterial clots, venous clots, and pulmonary embolism.
Discussion: Our study supports existing literature regarding severe C. difficile with AKI as a risk factor for decompensation of liver disease and related mortality. Based on the findings of a result, we recommend a lower threshold for treatment of CDI in patients with cirrhosis and diarrhea of unknown etiology and limit unnecessary exposure to antibiotics to decrease risk of CDI.
Disclosures:
Het Patel, DO1, Naomi Reddy-Patel, MD2, Zarian Prenatt, DO1, Hammad Liaquat, MD2. P0175 - Assessing Acute Kidney Injury in Patients With Cirrhosis and Clostridium difficile Infection: A 5-Year National Inpatient Sample Analysis of Hospital Complications, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Clostridium Difficile Infection (CDI) has a greater incidence in patients with liver cirrhosis for multiple reasons such as recurrent hospitalizations, immunodeficiency, and long-term antibiotic use. Cirrhosis also has profound effects on the body’s baseline hemodynamics and renin-angiogenin-aldosterone system. The aim of the study is to assess the risk of adverse outcomes of acute kidney injury (AKI) in patients with CDI and cirrhosis.
Methods: This is a retrospective cohort study using National Inpatient Sample data including adults with history of liver cirrhosis hospitalized between 2016 and 2020 presenting with CDI. The primary outcome measured was inpatient complications in patients with AKI. Statistical analyses were all performed using STATA software.
Results: Of the 28,415 patients with cirrhosis who presented with CDI, 11,095 (39%) patients had AKI of which 56.7% were males and 68.1% were Caucasian. Patients with class obesity 3, malnutrition, length of stay and Charlson Comorbidity Index (CCI) of 5 or more had statistically significant (p< 0.05) association with AKI while CCI of 3 or less and smoking history was protective (Table 1). Patients with AKI were associated with ascites (OR=1.691; 95% CI 1.518-1.883), SBP (OR=2.534; 95% CI 1.937-3.316), hepatic encephalopathy (OR=3.092; 95% CI 1.848-5.172), acute liver failure (OR=2.827; 95% CI 2.159-3.703), acute respiratory failure (OR=3.176; 95% CI 2.738-3.681), shock (OR=4.655; 95% CI 3.844-5.637), and mortality (OR=4.695; 95% CI 3.839-5.743). Patients with AKI were also associated with increased requirement of blood transfusion (OR=1.868; 95% CI 1.605-2.173), intubation (OR=3.999; 95% CI 3.309-4.832), vasopressors (OR=3.927; 95% CI 2.579-5.981), and ICU level of care (OR=3.663; 95% CI 3.111-4.312) (Table 2). Patients with PBC did not have a statistically significant association (p >0.05) with variceal bleed, arterial clots, venous clots, and pulmonary embolism.
Discussion: Our study supports existing literature regarding severe C. difficile with AKI as a risk factor for decompensation of liver disease and related mortality. Based on the findings of a result, we recommend a lower threshold for treatment of CDI in patients with cirrhosis and diarrhea of unknown etiology and limit unnecessary exposure to antibiotics to decrease risk of CDI.
Table: Demographics and Length of Stay (Table 1) and inpatient complication (Table 2) of patients with cirrhosis and Clostridium Difficile Infection (CDI) in patients with AKI versus without AKI from 2016 to 2020.
Abbreviations: AKI = Acute Kidney Injury, SBP = Spontaneous Bacterial Peritonitis, ICU = Intensive Care Unit
Abbreviations: AKI = Acute Kidney Injury, SBP = Spontaneous Bacterial Peritonitis, ICU = Intensive Care Unit
Disclosures:
Het Patel indicated no relevant financial relationships.
Naomi Reddy-Patel indicated no relevant financial relationships.
Zarian Prenatt indicated no relevant financial relationships.
Hammad Liaquat indicated no relevant financial relationships.
Het Patel, DO1, Naomi Reddy-Patel, MD2, Zarian Prenatt, DO1, Hammad Liaquat, MD2. P0175 - Assessing Acute Kidney Injury in Patients With Cirrhosis and Clostridium difficile Infection: A 5-Year National Inpatient Sample Analysis of Hospital Complications, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
