Sunday Poster Session
Category: Colon
P0254 - A Case of Suspected Adult Eosinophilic Colitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jonathan Hansen, DO
Kirk Kerkorian School of Medicine at UNLV
Las Vegas, NV
Presenting Author(s)
Jonathan Hansen, DO1, Kyaw Min Tun, DO1, Rajan Amin, MD2, Jose Aponte-Pieras, MD1, Gordon Ohning, MD, PhD1
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2University of Nevada, Las Vegas, Las Vegas, NV
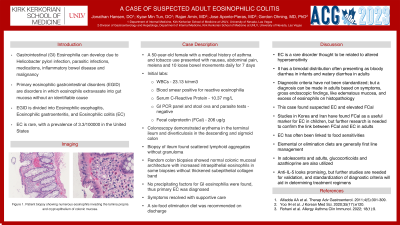
Introduction: Gastrointestinal (GI) Eosinophilia can develop due to many known causes such as Helicobacter pylori infection, parasitic infections, medications, inflammatory bowel disease and malignancy. Primary eosinophilic gastrointestinal disorders (EGID) are disorders in which eosinophils extravasate into gut mucosa without an identifiable cause. EGID is divided into Eosinophilic esophagitis, Eosinophilic gastroenteritis, and Eosinophilic colitis (EC). EC is rare with a prevalence of 3.3/100000 in the United States.
Case Description/Methods: A 50-year-old female with a medical history of asthma and tobacco use presented with nausea, abdominal pain, melena and 10 loose bowel movements daily for 7 days. Initial labs showed WBCs of 23.13 k/mm3 and a blood smear positive for reactive eosinophilia. Serum C-Reactive Protein level was also elevated at 10.37 mg/L. GI PCR panel and stool ova and parasite tests were negative. Fecal calprotectin (FCal) was 206 ug/g. A subsequent colonoscopy demonstrated erythema in the terminal ileum and diverticulosis in the descending and sigmoid colon. Biopsy of ileum found scattered lymphoid aggregates without granuloma. Random colon biopsies showed normal colonic mucosal architecture with increased intraepithelial eosinophils in some biopsies without thickened subepithelial collagen band. No precipitating factors for GI eosinophilia were found, thus primary EC was diagnosed. The patient’s symptoms resolved with supportive care and a six-food elimination diet was recommended on discharge.
Discussion: EC is a rare disorder thought to be related to altered hypersensitivity. It has a bimodal distribution often presenting as bloody diarrhea in infants and watery diarrhea in adults. Diagnostic criteria have not been standardized; but a diagnosis can be made in adults based on symptoms, gross endoscopic findings like edematous mucosa and excess of eosinophils on histopathology. This case found suspected EC and elevated FCal. Studies in Korea and Iran have found FCal as a useful marker for EC in children. Further research is needed to confirm the link between FCal and EC in adults. As EC has often been linked to food sensitivities, elemental or elimination diets are generally first line management. However, in adolescents and adults, glucocorticoids and azathioprine are often utilized. Novel approaches with IL-5 look promising, but further studies are needed for validation. Standardization of diagnostic criteria will aid in determining which patients need these options of treatment.
Disclosures:
Jonathan Hansen, DO1, Kyaw Min Tun, DO1, Rajan Amin, MD2, Jose Aponte-Pieras, MD1, Gordon Ohning, MD, PhD1. P0254 - A Case of Suspected Adult Eosinophilic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Gastrointestinal (GI) Eosinophilia can develop due to many known causes such as Helicobacter pylori infection, parasitic infections, medications, inflammatory bowel disease and malignancy. Primary eosinophilic gastrointestinal disorders (EGID) are disorders in which eosinophils extravasate into gut mucosa without an identifiable cause. EGID is divided into Eosinophilic esophagitis, Eosinophilic gastroenteritis, and Eosinophilic colitis (EC). EC is rare with a prevalence of 3.3/100000 in the United States.
Case Description/Methods: A 50-year-old female with a medical history of asthma and tobacco use presented with nausea, abdominal pain, melena and 10 loose bowel movements daily for 7 days. Initial labs showed WBCs of 23.13 k/mm3 and a blood smear positive for reactive eosinophilia. Serum C-Reactive Protein level was also elevated at 10.37 mg/L. GI PCR panel and stool ova and parasite tests were negative. Fecal calprotectin (FCal) was 206 ug/g. A subsequent colonoscopy demonstrated erythema in the terminal ileum and diverticulosis in the descending and sigmoid colon. Biopsy of ileum found scattered lymphoid aggregates without granuloma. Random colon biopsies showed normal colonic mucosal architecture with increased intraepithelial eosinophils in some biopsies without thickened subepithelial collagen band. No precipitating factors for GI eosinophilia were found, thus primary EC was diagnosed. The patient’s symptoms resolved with supportive care and a six-food elimination diet was recommended on discharge.
Discussion: EC is a rare disorder thought to be related to altered hypersensitivity. It has a bimodal distribution often presenting as bloody diarrhea in infants and watery diarrhea in adults. Diagnostic criteria have not been standardized; but a diagnosis can be made in adults based on symptoms, gross endoscopic findings like edematous mucosa and excess of eosinophils on histopathology. This case found suspected EC and elevated FCal. Studies in Korea and Iran have found FCal as a useful marker for EC in children. Further research is needed to confirm the link between FCal and EC in adults. As EC has often been linked to food sensitivities, elemental or elimination diets are generally first line management. However, in adolescents and adults, glucocorticoids and azathioprine are often utilized. Novel approaches with IL-5 look promising, but further studies are needed for validation. Standardization of diagnostic criteria will aid in determining which patients need these options of treatment.
Disclosures:
Jonathan Hansen indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Gordon Ohning indicated no relevant financial relationships.
Jonathan Hansen, DO1, Kyaw Min Tun, DO1, Rajan Amin, MD2, Jose Aponte-Pieras, MD1, Gordon Ohning, MD, PhD1. P0254 - A Case of Suspected Adult Eosinophilic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
