Sunday Poster Session
Category: Colon
P0286 - An Interesting Case of Microscopic Colitis Flare Induced by Diuretics and ACE-I
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Alaa Taha, MD
Wayne State University/Ascension Providence Rochester Hospital
Rochester, MI
Presenting Author(s)
Shahed Hussein, MD1, Warda Zaidi, MD2, Alaa Taha, MD2, Hasan Ilyas, MD2, Tony Calabrese, MD2, Vesna Tegeltija, MD2
1Wayne State University School of Medicine, Rochester, MI; 2Wayne State University GME, Rochester, MI
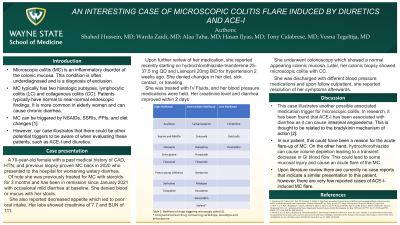
Introduction: Microscopic colitis (MC) is an inflammatory disorder of the colonic mucosa. This condition is often underdiagnosed and is a diagnosis of exclusion. Patients typically have normal to near-normal endoscopic findings. MC typically consists of lymphocytic colitis (LC) and collagenous colitis (CC). It is more common in elderly women and can cause chronic diarrhea. MC can be triggered by NSAIDs, SSRIs, PPIs, and diet changes. However, our case illustrates that there could be other potential triggers to be aware of when evaluating these patients, such as ACE-I and diuretics.
Case Description/Methods: A 70-year-old female presented with a PMHx of CAD, HTN, and previous biopsy-proven MC back in 2020. She was treated with steroids for 3 months and in remission since January 2021 with occasional mild diarrhea at baseline. In her current presentation, she had worsening watery diarrhea with no blood or mucus. She also reported decreased appetite which led to poor oral intake. Her lab showed creatinine of 7.7 and BUN of 111. Further review of her medication, she reported recently starting on hydrochlorothiazide-triamterene 25-37.5mg QD and Lisinopril 20mg BID for hypertension which she was on for 2 weeks. She denies changes in her diet, sick contact, or traveling. We treated her with IV Fluids, and BP medications were held. Her creatinine level and diarrhea improved within 2 days. She underwent with colonoscopy Which showed normal appearing colonic mucosa. Later, her colonic biopsy showed microscopic colitis with CC. She was discharged with new blood pressure medication and outpatient follow-up reported resolution of her symptoms.
Discussion: This case illustrates another possible associated medication trigger for microscopic colitis. In research, it has been found that ACE-I has been associated with diarrhea as it can cause intestinal angioedema. This is thought to be related to the bradykinin mechanism of action. In our patient, this could have been a reason for the acute flare-up of MC. On the other hand, hydrochlorothiazide can cause volume depletion leading to a transient decrease in GI blood flow. This could lead to some mucosal injury and cause an acute flare of the MC. Upon literature review there are currently no case reports that indicate a similar presentation to this patient, however, there are very few reported cases of ACE-I-induced MC flare.
Disclosures:
Shahed Hussein, MD1, Warda Zaidi, MD2, Alaa Taha, MD2, Hasan Ilyas, MD2, Tony Calabrese, MD2, Vesna Tegeltija, MD2. P0286 - An Interesting Case of Microscopic Colitis Flare Induced by Diuretics and ACE-I, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University School of Medicine, Rochester, MI; 2Wayne State University GME, Rochester, MI
Introduction: Microscopic colitis (MC) is an inflammatory disorder of the colonic mucosa. This condition is often underdiagnosed and is a diagnosis of exclusion. Patients typically have normal to near-normal endoscopic findings. MC typically consists of lymphocytic colitis (LC) and collagenous colitis (CC). It is more common in elderly women and can cause chronic diarrhea. MC can be triggered by NSAIDs, SSRIs, PPIs, and diet changes. However, our case illustrates that there could be other potential triggers to be aware of when evaluating these patients, such as ACE-I and diuretics.
Case Description/Methods: A 70-year-old female presented with a PMHx of CAD, HTN, and previous biopsy-proven MC back in 2020. She was treated with steroids for 3 months and in remission since January 2021 with occasional mild diarrhea at baseline. In her current presentation, she had worsening watery diarrhea with no blood or mucus. She also reported decreased appetite which led to poor oral intake. Her lab showed creatinine of 7.7 and BUN of 111. Further review of her medication, she reported recently starting on hydrochlorothiazide-triamterene 25-37.5mg QD and Lisinopril 20mg BID for hypertension which she was on for 2 weeks. She denies changes in her diet, sick contact, or traveling. We treated her with IV Fluids, and BP medications were held. Her creatinine level and diarrhea improved within 2 days. She underwent with colonoscopy Which showed normal appearing colonic mucosa. Later, her colonic biopsy showed microscopic colitis with CC. She was discharged with new blood pressure medication and outpatient follow-up reported resolution of her symptoms.
Discussion: This case illustrates another possible associated medication trigger for microscopic colitis. In research, it has been found that ACE-I has been associated with diarrhea as it can cause intestinal angioedema. This is thought to be related to the bradykinin mechanism of action. In our patient, this could have been a reason for the acute flare-up of MC. On the other hand, hydrochlorothiazide can cause volume depletion leading to a transient decrease in GI blood flow. This could lead to some mucosal injury and cause an acute flare of the MC. Upon literature review there are currently no case reports that indicate a similar presentation to this patient, however, there are very few reported cases of ACE-I-induced MC flare.
Disclosures:
Shahed Hussein indicated no relevant financial relationships.
Warda Zaidi indicated no relevant financial relationships.
Alaa Taha indicated no relevant financial relationships.
Hasan Ilyas indicated no relevant financial relationships.
Tony Calabrese indicated no relevant financial relationships.
Vesna Tegeltija indicated no relevant financial relationships.
Shahed Hussein, MD1, Warda Zaidi, MD2, Alaa Taha, MD2, Hasan Ilyas, MD2, Tony Calabrese, MD2, Vesna Tegeltija, MD2. P0286 - An Interesting Case of Microscopic Colitis Flare Induced by Diuretics and ACE-I, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
