Sunday Poster Session
Category: Colon
P0312 - Emerging Diagnostic Markers in Acute Ischemic Colitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Hassan Zreik, MD
Henry Ford Health System
Jackson, Michigan
Presenting Author(s)
Hassan Zreik, MD1, Bipneet Singh, MD2, Parth M. Patel, MD3, Zarqa Yasin, MD2, Parneet Hari, MD4, Chidamber Bharath Alamelumangapuram, MD4
1Henry Ford Health System, Jackson, MI; 2Henry Ford Health, Jackson, MI; 3Henry Ford Health System, Boston, MA; 4Henry Ford Jackson, Jackson, MI
Introduction: Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting older adults. The incidence is estimated at 16 cases per 100,000 person-years, which has increased over time. Colonic ischemia should be suspected in patients admitted for heart failure with lower abdominal pain and bloody diarrhea or hematochezia.
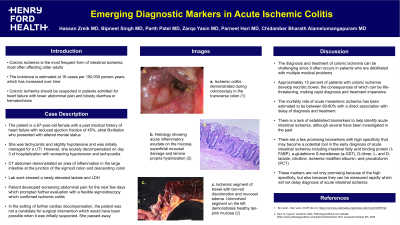
Case Description/Methods: The patient is a 67-year-old female with past medical history of heart failure with reduced ejection fraction of 45%, atrial fibrillation who presented with altered mental status. Patient's neurological examination was unrevealing. Patient was tachycardic and slightly hypotensive. Patient was initially managed for a UTI, however acutely decompensated on day 3 of hospitalization. Hypotension and tachycardia significantly worsened. A stat CT abdomen demonstrated an area of inflammation in the large intestine at the junction of sigmoid colon and descending colon. Lab work showed a newly elevated lactate and LDH. General surgery was consulted and recommended continued observation given their assessment of a benign physical exam. Patient developed worsening abdominal pain for the next few days which prompted further evaluation with a flexible sigmoidoscopy which confirmed ischemic colitis. In the setting of further cardiac decompensation, the patient was not a candidate for surgical intervention which would have been possible when it was suspected and passed away.
Discussion: The diagnosis and treatment of colonic ischemia can be challenging since it often occurs in patients who are debilitated with multiple medical problems. Approximately 15 percent of patients with colonic ischemia develop necrotic bowel, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. There is a lack of established biomarkers to help identify acute intestinal ischemia, although several have been investigated in the past. There is a few promising biomarkers with high specificity that may become a potential tool in early diagnosis of acute intestinal ischemia including intestinal fatty acid binding protein (I-FABP), a-glutathione S-transferase (a-GST), D-dimer, L- and D-lactate, citrulline, ischemia modified albumin, and procalcitonin (PCT). These markers are not only promising because of the high specificity, but also because they can be measured rapidly which will not delay diagnosis of acute intestinal ischemia.
Disclosures:
Hassan Zreik, MD1, Bipneet Singh, MD2, Parth M. Patel, MD3, Zarqa Yasin, MD2, Parneet Hari, MD4, Chidamber Bharath Alamelumangapuram, MD4. P0312 - Emerging Diagnostic Markers in Acute Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Health System, Jackson, MI; 2Henry Ford Health, Jackson, MI; 3Henry Ford Health System, Boston, MA; 4Henry Ford Jackson, Jackson, MI
Introduction: Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting older adults. The incidence is estimated at 16 cases per 100,000 person-years, which has increased over time. Colonic ischemia should be suspected in patients admitted for heart failure with lower abdominal pain and bloody diarrhea or hematochezia.
Case Description/Methods: The patient is a 67-year-old female with past medical history of heart failure with reduced ejection fraction of 45%, atrial fibrillation who presented with altered mental status. Patient's neurological examination was unrevealing. Patient was tachycardic and slightly hypotensive. Patient was initially managed for a UTI, however acutely decompensated on day 3 of hospitalization. Hypotension and tachycardia significantly worsened. A stat CT abdomen demonstrated an area of inflammation in the large intestine at the junction of sigmoid colon and descending colon. Lab work showed a newly elevated lactate and LDH. General surgery was consulted and recommended continued observation given their assessment of a benign physical exam. Patient developed worsening abdominal pain for the next few days which prompted further evaluation with a flexible sigmoidoscopy which confirmed ischemic colitis. In the setting of further cardiac decompensation, the patient was not a candidate for surgical intervention which would have been possible when it was suspected and passed away.
Discussion: The diagnosis and treatment of colonic ischemia can be challenging since it often occurs in patients who are debilitated with multiple medical problems. Approximately 15 percent of patients with colonic ischemia develop necrotic bowel, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. There is a lack of established biomarkers to help identify acute intestinal ischemia, although several have been investigated in the past. There is a few promising biomarkers with high specificity that may become a potential tool in early diagnosis of acute intestinal ischemia including intestinal fatty acid binding protein (I-FABP), a-glutathione S-transferase (a-GST), D-dimer, L- and D-lactate, citrulline, ischemia modified albumin, and procalcitonin (PCT). These markers are not only promising because of the high specificity, but also because they can be measured rapidly which will not delay diagnosis of acute intestinal ischemia.
Disclosures:
Hassan Zreik indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Zarqa Yasin indicated no relevant financial relationships.
Parneet Hari indicated no relevant financial relationships.
Chidamber Bharath Alamelumangapuram indicated no relevant financial relationships.
Hassan Zreik, MD1, Bipneet Singh, MD2, Parth M. Patel, MD3, Zarqa Yasin, MD2, Parneet Hari, MD4, Chidamber Bharath Alamelumangapuram, MD4. P0312 - Emerging Diagnostic Markers in Acute Ischemic Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
