Sunday Poster Session
Category: Colon
P0314 - Mpox Virus-Associated Severe Proctitis in a Young Male
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aishwarya Thakurdesai, MBBS, MD
University of Louisville School of Medicine
Louisville, KY
Presenting Author(s)
Aishwarya Thakurdesai, MBBS, MD, Steven Edds, DO, Adam Hoehn, DO, Kartik Garg, BS, Endashaw Omer, MD, MPH, FACG
University of Louisville School of Medicine, Louisville, KY
Introduction: An outbreak of mpox involving multiple nonendemic countries was identified in May 2022. Cases have been reported mainly among males aged 18-50 years, and men who have sex with men (MSM). The clinical features of mpox in the current outbreak are widely different from earlier descriptions. Specifically, patients present with symptoms like a rash in the anogenital regions, proctitis, and severe anorectal pain. Here, we report a case of severe proctitis in a young male who tested positive for mpox.
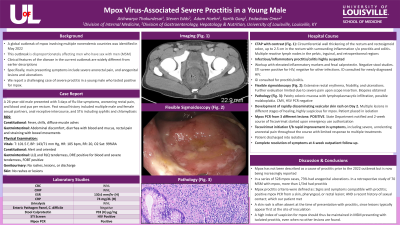
Case Description/Methods: A 26-year-old male with a past medical history of syphilis presented with 3 days of flu-like symptoms, rectal pain, and blood and pus per rectum. He had a history of multiple male and female sexual partners. Infectious proctitis was suspected based on the patient’s age, symptoms, and high-risk sexual history. Workup was positive for HIV, but negative for other infections. Antiretroviral therapy was initiated. A CT scan revealed circumferential wall thickening of the rectum and rectosigmoid colon, suggestive of proctitis and colitis. A flexible sigmoidoscopy demonstrated extensive rectal erythema, friability, and ulcerations. Severe pain upon insertion of the scope limited further colonic evaluation. Pathology showed patchy colonic mucosa with lymphoplasmacytic infiltration. Possible malakoplakia was also seen. CMV and HSV tests were negative. The patient developed a skin rash on the 2nd day of hospitalization. It rapidly disseminated to areas including the anogenital area, with multiple lesions in different stages of healing. Swabs from 3 different lesions tested positive for mpox PCR. Throughout his hospital course, the patient experienced severe anorectal pain which did not improve with topical analgesics or mesalamine suppositories. A 2-week course of tecovirimat was started and the patient was discharged into isolation. At 4-week follow-up, all of his symptoms had completely resolved.
Discussion: Mpox has not been described as a cause of proctitis prior to the 2022 outbreak but is now being increasingly reported. In a chart review of 70 MSM with mpox, more than 1/3rd had proctitis. Mpox proctitis criteria were defined as signs and symptoms compatible with proctitis; positive mpox PCR from a skin, pharyngeal, or rectal lesion; and a recent history of sexual contact; which our patient met. A rash is often absent at the time of presentation with proctitis, as with our case. Thus, mpox should be suspected in MSM presenting with proctitis, even if no other lesions are found.

Disclosures:
Aishwarya Thakurdesai, MBBS, MD, Steven Edds, DO, Adam Hoehn, DO, Kartik Garg, BS, Endashaw Omer, MD, MPH, FACG. P0314 - Mpox Virus-Associated Severe Proctitis in a Young Male, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Louisville School of Medicine, Louisville, KY
Introduction: An outbreak of mpox involving multiple nonendemic countries was identified in May 2022. Cases have been reported mainly among males aged 18-50 years, and men who have sex with men (MSM). The clinical features of mpox in the current outbreak are widely different from earlier descriptions. Specifically, patients present with symptoms like a rash in the anogenital regions, proctitis, and severe anorectal pain. Here, we report a case of severe proctitis in a young male who tested positive for mpox.
Case Description/Methods: A 26-year-old male with a past medical history of syphilis presented with 3 days of flu-like symptoms, rectal pain, and blood and pus per rectum. He had a history of multiple male and female sexual partners. Infectious proctitis was suspected based on the patient’s age, symptoms, and high-risk sexual history. Workup was positive for HIV, but negative for other infections. Antiretroviral therapy was initiated. A CT scan revealed circumferential wall thickening of the rectum and rectosigmoid colon, suggestive of proctitis and colitis. A flexible sigmoidoscopy demonstrated extensive rectal erythema, friability, and ulcerations. Severe pain upon insertion of the scope limited further colonic evaluation. Pathology showed patchy colonic mucosa with lymphoplasmacytic infiltration. Possible malakoplakia was also seen. CMV and HSV tests were negative. The patient developed a skin rash on the 2nd day of hospitalization. It rapidly disseminated to areas including the anogenital area, with multiple lesions in different stages of healing. Swabs from 3 different lesions tested positive for mpox PCR. Throughout his hospital course, the patient experienced severe anorectal pain which did not improve with topical analgesics or mesalamine suppositories. A 2-week course of tecovirimat was started and the patient was discharged into isolation. At 4-week follow-up, all of his symptoms had completely resolved.
Discussion: Mpox has not been described as a cause of proctitis prior to the 2022 outbreak but is now being increasingly reported. In a chart review of 70 MSM with mpox, more than 1/3rd had proctitis. Mpox proctitis criteria were defined as signs and symptoms compatible with proctitis; positive mpox PCR from a skin, pharyngeal, or rectal lesion; and a recent history of sexual contact; which our patient met. A rash is often absent at the time of presentation with proctitis, as with our case. Thus, mpox should be suspected in MSM presenting with proctitis, even if no other lesions are found.

Figure: CT scan demonstrating significant circumferential wall thickening of the rectum, suggestive of severe proctitis
Disclosures:
Aishwarya Thakurdesai indicated no relevant financial relationships.
Steven Edds indicated no relevant financial relationships.
Adam Hoehn indicated no relevant financial relationships.
Kartik Garg indicated no relevant financial relationships.
Endashaw Omer indicated no relevant financial relationships.
Aishwarya Thakurdesai, MBBS, MD, Steven Edds, DO, Adam Hoehn, DO, Kartik Garg, BS, Endashaw Omer, MD, MPH, FACG. P0314 - Mpox Virus-Associated Severe Proctitis in a Young Male, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

