Sunday Poster Session
Category: Colon
P0317 - Intestinal Tuberculosis Presenting as Increased Abdominal Girth and Recurrent Fevers
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Ixel Cervera, MD
NYU Langone Hospital-Brooklyn
New York, NY
Presenting Author(s)
Ixel Cervera, MD1, Navina Mohan, MD1, Morris Jrada, MD1, Lalitha Parameswaran, MD, MPH1, Saikiran Kilaru, MD2
1NYU Langone Hospital-Brooklyn, Brooklyn, NY; 2NYU Langone Hospital, New York, NY
Introduction: Intestinal tuberculosis (TB) is the sixth most common site of extrapulmonary TB. Diagnosis requires a high degree of suspicion due to non-specific symptoms that may mimic other abdominal pathologies caused by inflammatory disease, infections, and malignancies.
Case Description/Methods: A 40 year old man from Mexico with EtOH use disorder presented with painful abdominal distention, dark tarry stools, sweating and tremors. Vitals were T100.9F HR 120 RR 22 BP 122/70 SpO2 99% on RA. Exam revealed cachexia and ascites, but no jaundice. Labs included lactate 3.75, Na 120, AST 200, ALT 48, Tbili 3, Dbili 2.2, albumin 2.8, LDH 304, INR 2.2, WBC 3.3, Hgb10.6, Hct30.8, Plt 75, procalcitonin 0.61. Diagnostic paracentesis showed 894 nucleated cells, 80% lymphocytes, 11% neutrophils equaling to 98 PMNs, with a SAAG of 1.5. CT abdomen revealed liver cirrhosis and 1cm hypoatenuating nodule. Infectious work up including HIV and hepatitis serologies, and blood and urine cultures were negative. Sputum AFB smears and ascitic fluid nucleic acid amplification test for Mycobacterium tuberculosis complex (MTB PCR) were all negative. A nuclear indium whole body scan was negative for occult infectious source. Leukemia/lymphoma panel was negative. Colonoscopy revealed blood in the cecum and two single solitary ulcers in the ileum with edematous mucosa. The distal ulcer was biopsied. Pathology showed chronic ileitis with necrotizing granulomas. Tissue culture was positive for AFB and MTB PCR. CT chest showed miliary nodules. He was started on rifampin, isoniazid, pyrazinamide and ethambutol (RIPE) for intestinal TB, and symptoms resolved.
Discussion: Extrapulmonary TB occurs in 15-20% of patients not infected with HIV, of which only 5% of case are intestinal. Difficulty in diagnosing intestinal TB stems from vague symptoms on presentation, as well as low suspicion when a patient is from a nonendemic country. Only about 15-25% of individuals with gastrointestinal TB have concomitant pulmonary TB. Delay in diagnosis can lead to complications such as bowel obstruction, perforation, stricture, abscess and/or fistula formation. Individuals placed on immunosuppressive therapy for presumed inflammatory bowel disease prior to TB diagnosis may develop systemic spread. B symptoms with abdominal symptoms should lead to malignancy and intestinal TB work up as early treatment affects morbidity and mortality. Colonoscopy with biopsy of intestinal findings can increase diagnostic yield.

Disclosures:
Ixel Cervera, MD1, Navina Mohan, MD1, Morris Jrada, MD1, Lalitha Parameswaran, MD, MPH1, Saikiran Kilaru, MD2. P0317 - Intestinal Tuberculosis Presenting as Increased Abdominal Girth and Recurrent Fevers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1NYU Langone Hospital-Brooklyn, Brooklyn, NY; 2NYU Langone Hospital, New York, NY
Introduction: Intestinal tuberculosis (TB) is the sixth most common site of extrapulmonary TB. Diagnosis requires a high degree of suspicion due to non-specific symptoms that may mimic other abdominal pathologies caused by inflammatory disease, infections, and malignancies.
Case Description/Methods: A 40 year old man from Mexico with EtOH use disorder presented with painful abdominal distention, dark tarry stools, sweating and tremors. Vitals were T100.9F HR 120 RR 22 BP 122/70 SpO2 99% on RA. Exam revealed cachexia and ascites, but no jaundice. Labs included lactate 3.75, Na 120, AST 200, ALT 48, Tbili 3, Dbili 2.2, albumin 2.8, LDH 304, INR 2.2, WBC 3.3, Hgb10.6, Hct30.8, Plt 75, procalcitonin 0.61. Diagnostic paracentesis showed 894 nucleated cells, 80% lymphocytes, 11% neutrophils equaling to 98 PMNs, with a SAAG of 1.5. CT abdomen revealed liver cirrhosis and 1cm hypoatenuating nodule. Infectious work up including HIV and hepatitis serologies, and blood and urine cultures were negative. Sputum AFB smears and ascitic fluid nucleic acid amplification test for Mycobacterium tuberculosis complex (MTB PCR) were all negative. A nuclear indium whole body scan was negative for occult infectious source. Leukemia/lymphoma panel was negative. Colonoscopy revealed blood in the cecum and two single solitary ulcers in the ileum with edematous mucosa. The distal ulcer was biopsied. Pathology showed chronic ileitis with necrotizing granulomas. Tissue culture was positive for AFB and MTB PCR. CT chest showed miliary nodules. He was started on rifampin, isoniazid, pyrazinamide and ethambutol (RIPE) for intestinal TB, and symptoms resolved.
Discussion: Extrapulmonary TB occurs in 15-20% of patients not infected with HIV, of which only 5% of case are intestinal. Difficulty in diagnosing intestinal TB stems from vague symptoms on presentation, as well as low suspicion when a patient is from a nonendemic country. Only about 15-25% of individuals with gastrointestinal TB have concomitant pulmonary TB. Delay in diagnosis can lead to complications such as bowel obstruction, perforation, stricture, abscess and/or fistula formation. Individuals placed on immunosuppressive therapy for presumed inflammatory bowel disease prior to TB diagnosis may develop systemic spread. B symptoms with abdominal symptoms should lead to malignancy and intestinal TB work up as early treatment affects morbidity and mortality. Colonoscopy with biopsy of intestinal findings can increase diagnostic yield.

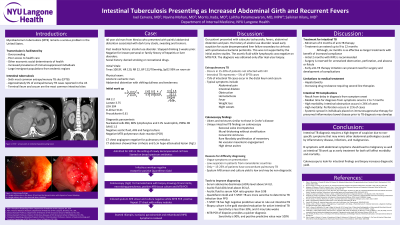
Figure: Colonoscopy Findings:
a. A single solitary ulcer in the ileum, 10 cm from the ileocecal valve, with stigmata of recent bleeding
b. A single solitary ulcer in the terminal ileum, biopsied
a. A single solitary ulcer in the ileum, 10 cm from the ileocecal valve, with stigmata of recent bleeding
b. A single solitary ulcer in the terminal ileum, biopsied
Disclosures:
Ixel Cervera indicated no relevant financial relationships.
Navina Mohan indicated no relevant financial relationships.
Morris Jrada indicated no relevant financial relationships.
Lalitha Parameswaran indicated no relevant financial relationships.
Saikiran Kilaru indicated no relevant financial relationships.
Ixel Cervera, MD1, Navina Mohan, MD1, Morris Jrada, MD1, Lalitha Parameswaran, MD, MPH1, Saikiran Kilaru, MD2. P0317 - Intestinal Tuberculosis Presenting as Increased Abdominal Girth and Recurrent Fevers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
