Sunday Poster Session
Category: Colon
P0319 - Hemorrhagic Colitis in a Patient With Granulomatosis With Polyangiitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DB
Daniel Burkholder, MD
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Daniel Burkholder, MD1, Christopher Fan, MD2
1Houston Methodist Hospital, Houston, TX; 2Houston Methodist-Weill Cornell, Houston, TX
Introduction: Granulomatosis with polyangiitis (GPA) is an autoimmune condition characterized by the inflammation of small blood vessels. It most commonly affects the lungs, upper airway, and kidneys though uncommonly can affect the gastrointestinal (GI) tract. We describe a case of a middle-aged woman with GPA with prior small bowel involvement presenting with severe colitis.
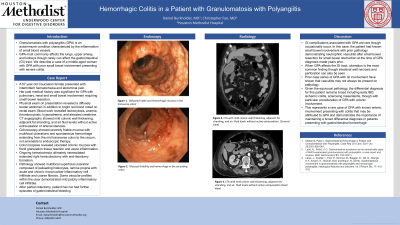
Case Description/Methods: A 57 year old Caucasian female presented with intermittent hematochezia and abdominal pain. Her past medical history was significant for GPA with pulmonary, renal and small bowel involvement requiring small bowel resection. Physical exam revealed a diffusely tender abdomen in addition to bright red blood noted on rectal exam. Blood work revealed leukocytosis, anemia, thrombocytosis, hyponatremia, and elevated creatinine. Colonoscopy showed severely friable mucosa with multifocal ulcerations and spontaneous hemorrhage extending from the mid transverse colon to the cecum, not amenable to endoscopic therapy. Biopsy showed ulcerated colonic mucosa with florid granulation tissue reaction and acute inflammation. The patient experienced continued significant hematochezia ultimately requiring extended right hemicolectomy with end-ileostomy formation. Pathology showed multifocal superficial ulceration composed of palisading histiocytes, lamina propria with acute and chronic mononuclear inflammatory cell infiltrate and coarse fibrosis. Some vascular profiles within the ulcer demonstrated mild patchy inflammatory cell infiltrate.
Discussion: GI complications associated with GPA are rare though occasionally occur. In this case, the patient had known small bowel involvement with prior pathology demonstrating neutrophilic vasculitis after small bowel resection for small bowel obstruction at the time of GPA diagnosis made years prior. When GPA affects the GI tract, ulceration is the most common finding though intestinal wall necrosis and perforation can also be seen. Prior case series of GPA with GI involvement have shown that vasculitis may not always be present on pathology. Given the equivocal pathology, the differential diagnosis for this patient remains broad including early IBD, ischemic colitis, sclerosing mesenteritis, though with particular consideration of GPA with colonic involvement. This represents a rare case of GPA with known enteric involvement presenting with colitis that may be attributed to GPA.

Disclosures:
Daniel Burkholder, MD1, Christopher Fan, MD2. P0319 - Hemorrhagic Colitis in a Patient With Granulomatosis With Polyangiitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Houston Methodist Hospital, Houston, TX; 2Houston Methodist-Weill Cornell, Houston, TX
Introduction: Granulomatosis with polyangiitis (GPA) is an autoimmune condition characterized by the inflammation of small blood vessels. It most commonly affects the lungs, upper airway, and kidneys though uncommonly can affect the gastrointestinal (GI) tract. We describe a case of a middle-aged woman with GPA with prior small bowel involvement presenting with severe colitis.
Case Description/Methods: A 57 year old Caucasian female presented with intermittent hematochezia and abdominal pain. Her past medical history was significant for GPA with pulmonary, renal and small bowel involvement requiring small bowel resection. Physical exam revealed a diffusely tender abdomen in addition to bright red blood noted on rectal exam. Blood work revealed leukocytosis, anemia, thrombocytosis, hyponatremia, and elevated creatinine. Colonoscopy showed severely friable mucosa with multifocal ulcerations and spontaneous hemorrhage extending from the mid transverse colon to the cecum, not amenable to endoscopic therapy. Biopsy showed ulcerated colonic mucosa with florid granulation tissue reaction and acute inflammation. The patient experienced continued significant hematochezia ultimately requiring extended right hemicolectomy with end-ileostomy formation. Pathology showed multifocal superficial ulceration composed of palisading histiocytes, lamina propria with acute and chronic mononuclear inflammatory cell infiltrate and coarse fibrosis. Some vascular profiles within the ulcer demonstrated mild patchy inflammatory cell infiltrate.
Discussion: GI complications associated with GPA are rare though occasionally occur. In this case, the patient had known small bowel involvement with prior pathology demonstrating neutrophilic vasculitis after small bowel resection for small bowel obstruction at the time of GPA diagnosis made years prior. When GPA affects the GI tract, ulceration is the most common finding though intestinal wall necrosis and perforation can also be seen. Prior case series of GPA with GI involvement have shown that vasculitis may not always be present on pathology. Given the equivocal pathology, the differential diagnosis for this patient remains broad including early IBD, ischemic colitis, sclerosing mesenteritis, though with particular consideration of GPA with colonic involvement. This represents a rare case of GPA with known enteric involvement presenting with colitis that may be attributed to GPA.

Figure: Endoscopic findings of diffusely friable and hemorrhagic colonic mucosa.
Disclosures:
Daniel Burkholder indicated no relevant financial relationships.
Christopher Fan indicated no relevant financial relationships.
Daniel Burkholder, MD1, Christopher Fan, MD2. P0319 - Hemorrhagic Colitis in a Patient With Granulomatosis With Polyangiitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
