Sunday Poster Session
Category: Colon
P0320 - Watch for Those Bumps! Yellow Nodules on Colonoscopy With Colonic Eosinophilia Leading to the Diagnosis of Strongyloidiasis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Arvin N. Tan, MD
University of Hawaii, John A. Burns School of Medicine
Honolulu, HI
Presenting Author(s)
Arvin Tan, MD1, Kristine Vo, MD1, Landon Kozai, MD1, Nigel Tourdot, MD1, Traci T. Murakami, MD2
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2Queen's Medical Center - West Oahu, Ewa Beach, HI
Introduction: Strongyloidiasis is a parasitic infection caused by roundworms endemic to tropical and subtropical regions. Infection is often asymptomatic or may present with nonspecific symptoms. Presented here are two cases of Strongyloidiasis diagnosed through findings of smooth yellow nodules on colonoscopy.
Case Description/Methods: We present two cases of Strongyloides infection discovered on routine screening colonoscopy after a biopsy of smooth round yellowish-white bumps revealed eosinophilia. Both patients were Filipino males who were born and raised in the Philippines and migrated to the US.
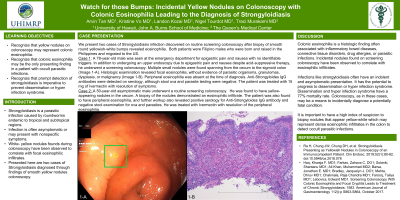
The first case is a 78-year-old male seen at the emergency department for epigastric pain and nausea with no identifiable triggers. In addition to undergoing an upper endoscopy due to epigastric pain and nausea despite acid-suppressive therapy, he underwent a screening colonoscopy. Multiple small nodules were found spanning from the cecum to the sigmoid colon (Image 1-A). Histologic examination revealed focal eosinophilia, without evidence of parasitic organisms, granulomas, dysplasia, or malignancy (Image I-B). Peripheral eosinophilia was absent at the time of diagnosis. Anti-Strongyloides IgG antibodies were detected on serology, although stool ova and parasite testing were negative. The patient was treated with 15 mg of Ivermectin with resolution of symptoms.
The second case is a 50-year-old asymptomatic male who underwent a routine screening colonoscopy. He was found to have yellow-appearing nodules in the cecum. A biopsy of the nodules demonstrated an eosinophilic infiltrate. The patient was also found to have peripheral eosinophilia, and further workup also revealed positive serology for Anti-Strongyloides IgG antibody and negative stool examination for ova and parasites. He was treated with Ivermectin with resolution of the peripheral eosinophilia.
Discussion: Colonic eosinophilia is a histologic finding often associated with inflammatory bowel diseases, connective tissue disorders, drug allergies, or parasitic infections. Since infections like strongyloidiasis have an indolent and asymptomatic presentation, colonoscopy, as in these cases, may be a means to diagnose a potentially fatal condition. Dissemination and hyperinfection syndrome have a 77% mortality rate. Thus, for patients at risk, it is important to have a high index of suspicion to biopsy yellow-white nodules that represent dense eosinophilic infiltrates in the colon to detect Strongyloidiasis and prevent hyperinfection syndrome.

Disclosures:
Arvin Tan, MD1, Kristine Vo, MD1, Landon Kozai, MD1, Nigel Tourdot, MD1, Traci T. Murakami, MD2. P0320 - Watch for Those Bumps! Yellow Nodules on Colonoscopy With Colonic Eosinophilia Leading to the Diagnosis of Strongyloidiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2Queen's Medical Center - West Oahu, Ewa Beach, HI
Introduction: Strongyloidiasis is a parasitic infection caused by roundworms endemic to tropical and subtropical regions. Infection is often asymptomatic or may present with nonspecific symptoms. Presented here are two cases of Strongyloidiasis diagnosed through findings of smooth yellow nodules on colonoscopy.
Case Description/Methods: We present two cases of Strongyloides infection discovered on routine screening colonoscopy after a biopsy of smooth round yellowish-white bumps revealed eosinophilia. Both patients were Filipino males who were born and raised in the Philippines and migrated to the US.
The first case is a 78-year-old male seen at the emergency department for epigastric pain and nausea with no identifiable triggers. In addition to undergoing an upper endoscopy due to epigastric pain and nausea despite acid-suppressive therapy, he underwent a screening colonoscopy. Multiple small nodules were found spanning from the cecum to the sigmoid colon (Image 1-A). Histologic examination revealed focal eosinophilia, without evidence of parasitic organisms, granulomas, dysplasia, or malignancy (Image I-B). Peripheral eosinophilia was absent at the time of diagnosis. Anti-Strongyloides IgG antibodies were detected on serology, although stool ova and parasite testing were negative. The patient was treated with 15 mg of Ivermectin with resolution of symptoms.
The second case is a 50-year-old asymptomatic male who underwent a routine screening colonoscopy. He was found to have yellow-appearing nodules in the cecum. A biopsy of the nodules demonstrated an eosinophilic infiltrate. The patient was also found to have peripheral eosinophilia, and further workup also revealed positive serology for Anti-Strongyloides IgG antibody and negative stool examination for ova and parasites. He was treated with Ivermectin with resolution of the peripheral eosinophilia.
Discussion: Colonic eosinophilia is a histologic finding often associated with inflammatory bowel diseases, connective tissue disorders, drug allergies, or parasitic infections. Since infections like strongyloidiasis have an indolent and asymptomatic presentation, colonoscopy, as in these cases, may be a means to diagnose a potentially fatal condition. Dissemination and hyperinfection syndrome have a 77% mortality rate. Thus, for patients at risk, it is important to have a high index of suspicion to biopsy yellow-white nodules that represent dense eosinophilic infiltrates in the colon to detect Strongyloidiasis and prevent hyperinfection syndrome.

Figure: 1-A: Smooth, yellow-white nodules on the colonic mucosa found on screening colonoscopy.
1-B: Colonic mucosa biopsy fragment exhibiting a dense eosinophilic infiltrate in the lamina propria, with eosinophilic cryptitis and microabscess, and crypt drop out. Additionally, there is granulation tissue and scattered chronic inflammatory cells.
1-B: Colonic mucosa biopsy fragment exhibiting a dense eosinophilic infiltrate in the lamina propria, with eosinophilic cryptitis and microabscess, and crypt drop out. Additionally, there is granulation tissue and scattered chronic inflammatory cells.
Disclosures:
Arvin Tan indicated no relevant financial relationships.
Kristine Vo indicated no relevant financial relationships.
Landon Kozai indicated no relevant financial relationships.
Nigel Tourdot indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Arvin Tan, MD1, Kristine Vo, MD1, Landon Kozai, MD1, Nigel Tourdot, MD1, Traci T. Murakami, MD2. P0320 - Watch for Those Bumps! Yellow Nodules on Colonoscopy With Colonic Eosinophilia Leading to the Diagnosis of Strongyloidiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
