Sunday Poster Session
Category: Colon
P0321 - Case Series: Critical Manifestations of Capecitabine-Induced Ileocolitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ana Rivera, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Sandra Gomez, MD, Ana Rivera, MD, Jiten Desai, MD, Paul Mustacchia, MD, MBA, Kaleem Rizvon, MD, Nausheer Khan, MD, Krishnaiyer Subramani, MD
Nassau University Medical Center, East Meadow, NY
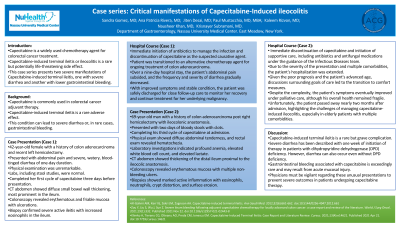
Introduction: Capecitabine can rarely induce terminal ileitis or ileocolitis that potentially leads to life-threatening outcomes. We present two cases of severe manifestations of Capecitabine-induced terminal ileocolitis.
Case Description/Methods: Case1:42-year-old female with a history of colon adenocarcinoma post left hemicolectomy presented with abdominal pain and severe watery blood-tinged diarrhea for one-day. Physical examination was unremarkable. Labs were within normal limits. She had completed her first cycle of capecitabine three-days prior to presentation. CT abdomen showed diffuse small bowel wall thickening predominantly in ileum. Colonoscopy showed erythematous,friable mucosa with ulcerations and exudates, suggestive of terminal ileitis. Biopsies revealed severe active ileitis with focal surface erosion and increased eosinophils. Patient was treated with antibiotics and Capecitabine was discontinued in favor of a different chemotherapy agent. She was discharged uneventfully on hospital day 9. Case2:69 year-old-man with history of colon adenocarcinoma post right hemicolectomy with ileocolonic anastomosis presented with two days of bloody stools with clots. He was completing his third cycle of capecitabine at prsentation. Physical exam was significant for diffuse abdominal tenderness and rectal exam positive for hematochezia. Labs showed anemia, leukocytosis and elevated lactate. CT abdomen showed thickening of distal ileum proximal to the ileocolic anastomosis. Colonoscopy revealed erythematous mucosa and multiple non-bleeding ulcers with exudates around ileocolonic anastomosis, proximally to the ileum. Biopsies showed marked active inflammation with lymphoblastic infiltrate, eosinophils, neutrophils, crypt distortion and surface erosion. Endoscopic diagnosis of capecitabine-induced ileocolitis was performed. Discontinuation of capecitabine in addition to supportive care was performed, and his symptoms eventually improved after a prolonged hospital course.
Discussion: Severe diarrhea has been described with one week of initiation of therapy in patients with dihydropyridine dehydrogenase (DPD) deficiency, however our patient had terminal ileitis within one week of starting capecitabine without DPD deficiency. Capecitabine-associated GI bleed is very rare, with a suggested mechanism based on loss of epithelial surface secondary to acute mucosal injury. Physicians should be aware of the rare but critical presentations of capecitabine-induced GI toxicity in order to prevent detrimental outcomes.
Disclosures:
Sandra Gomez, MD, Ana Rivera, MD, Jiten Desai, MD, Paul Mustacchia, MD, MBA, Kaleem Rizvon, MD, Nausheer Khan, MD, Krishnaiyer Subramani, MD. P0321 - Case Series: Critical Manifestations of Capecitabine-Induced Ileocolitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Capecitabine can rarely induce terminal ileitis or ileocolitis that potentially leads to life-threatening outcomes. We present two cases of severe manifestations of Capecitabine-induced terminal ileocolitis.
Case Description/Methods: Case1:42-year-old female with a history of colon adenocarcinoma post left hemicolectomy presented with abdominal pain and severe watery blood-tinged diarrhea for one-day. Physical examination was unremarkable. Labs were within normal limits. She had completed her first cycle of capecitabine three-days prior to presentation. CT abdomen showed diffuse small bowel wall thickening predominantly in ileum. Colonoscopy showed erythematous,friable mucosa with ulcerations and exudates, suggestive of terminal ileitis. Biopsies revealed severe active ileitis with focal surface erosion and increased eosinophils. Patient was treated with antibiotics and Capecitabine was discontinued in favor of a different chemotherapy agent. She was discharged uneventfully on hospital day 9. Case2:69 year-old-man with history of colon adenocarcinoma post right hemicolectomy with ileocolonic anastomosis presented with two days of bloody stools with clots. He was completing his third cycle of capecitabine at prsentation. Physical exam was significant for diffuse abdominal tenderness and rectal exam positive for hematochezia. Labs showed anemia, leukocytosis and elevated lactate. CT abdomen showed thickening of distal ileum proximal to the ileocolic anastomosis. Colonoscopy revealed erythematous mucosa and multiple non-bleeding ulcers with exudates around ileocolonic anastomosis, proximally to the ileum. Biopsies showed marked active inflammation with lymphoblastic infiltrate, eosinophils, neutrophils, crypt distortion and surface erosion. Endoscopic diagnosis of capecitabine-induced ileocolitis was performed. Discontinuation of capecitabine in addition to supportive care was performed, and his symptoms eventually improved after a prolonged hospital course.
Discussion: Severe diarrhea has been described with one week of initiation of therapy in patients with dihydropyridine dehydrogenase (DPD) deficiency, however our patient had terminal ileitis within one week of starting capecitabine without DPD deficiency. Capecitabine-associated GI bleed is very rare, with a suggested mechanism based on loss of epithelial surface secondary to acute mucosal injury. Physicians should be aware of the rare but critical presentations of capecitabine-induced GI toxicity in order to prevent detrimental outcomes.
Disclosures:
Sandra Gomez indicated no relevant financial relationships.
Ana Rivera indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Kaleem Rizvon indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Sandra Gomez, MD, Ana Rivera, MD, Jiten Desai, MD, Paul Mustacchia, MD, MBA, Kaleem Rizvon, MD, Nausheer Khan, MD, Krishnaiyer Subramani, MD. P0321 - Case Series: Critical Manifestations of Capecitabine-Induced Ileocolitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

