Sunday Poster Session
Category: Colorectal Cancer Prevention
P0333 - The Impact of the COVID-19 Pandemic on Colorectal Cancer Diagnosis by Screening Endoscopy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Anupama Ancha, MD
Baylor Scott & White Medical Center
Temple, TX
Presenting Author(s)
Anupama Ancha, MD1, Alexis Bejcek, MD1, Dania Bairuty, DO1, Kenneth Youens, MD2, Christopher Johnson, MD, PhD1
1Baylor Scott & White Medical Center, Temple, TX; 2BSWH, Round Rock, TX
Introduction: Colorectal cancer is a leading cause of morbidity and mortality, making up 10% of cancers and attributing to 9.4% of cancer deaths worldwide. Early detection of high-risk polyps by colonoscopy plays a key role in colorectal cancer surveillance.
The Covid-19 pandemic impacted many aspects of the healthcare system, including a reduction and, at times, a halt, in elective procedures such as screening colonoscopies. There has been a documented delay in the treatment of existing cancers and the screening and diagnosis of multiple types of cancer, including colorectal cancer.
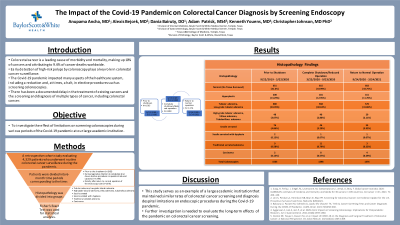
Methods: The objective of this study was to investigate the effect of limitations on screening colonoscopies during various periods of the Covid-19 pandemic at our large academic institution.
We conducted a retrospective cohort study evaluating 4,329 patients who underwent routine colorectal cancer surveillance during the pandemic. The patients were divided into 6-month time periods corresponding to the time prior to the shutdown (n=1565), the time during legislative direction to completely shut down elective procedures or operate at reduced capacity (n=1398), and the time directly after return to normal operation of the endoscopy suite (n=1376). We collected information on basic demographics, normal colonoscopies, and histopathology of tissue and polyps removed. Histopathology was divided into groups as follows: [tubular adenoma, low-grade tubular adenoma], [high-grade tubular adenoma, villous adenoma, tubulovillous adenoma], sessile serrated, sessile serrated with dysplasia, traditional serrated adenoma, and carcinoma.
Results: Using a Fisher’s Exact test, there was no significant difference in the detection of carcinoma- 0.13% (2/1565) prior to, 0.57% (8/1398) during, and 0.29% (4/1376) after the shutdown. There was also no significant difference in the rates of the groups of high-risk polyps that were investigated between the time periods. Overall, there was no significant difference in colon cancer surveillance and diagnosis in the time related to endoscopy suite shutdowns during the Covid-19 pandemic at this institution.
Discussion: This study serves as an example of a large academic institution that maintained similar rates of colorectal cancer screening and diagnosis despite limitations on endoscopic procedures during the Covid-19 pandemic. Further investigation is needed to evaluate the long-term effects of the pandemic on colorectal cancer screening.
Disclosures:
Anupama Ancha, MD1, Alexis Bejcek, MD1, Dania Bairuty, DO1, Kenneth Youens, MD2, Christopher Johnson, MD, PhD1. P0333 - The Impact of the COVID-19 Pandemic on Colorectal Cancer Diagnosis by Screening Endoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Temple, TX; 2BSWH, Round Rock, TX
Introduction: Colorectal cancer is a leading cause of morbidity and mortality, making up 10% of cancers and attributing to 9.4% of cancer deaths worldwide. Early detection of high-risk polyps by colonoscopy plays a key role in colorectal cancer surveillance.
The Covid-19 pandemic impacted many aspects of the healthcare system, including a reduction and, at times, a halt, in elective procedures such as screening colonoscopies. There has been a documented delay in the treatment of existing cancers and the screening and diagnosis of multiple types of cancer, including colorectal cancer.
Methods: The objective of this study was to investigate the effect of limitations on screening colonoscopies during various periods of the Covid-19 pandemic at our large academic institution.
We conducted a retrospective cohort study evaluating 4,329 patients who underwent routine colorectal cancer surveillance during the pandemic. The patients were divided into 6-month time periods corresponding to the time prior to the shutdown (n=1565), the time during legislative direction to completely shut down elective procedures or operate at reduced capacity (n=1398), and the time directly after return to normal operation of the endoscopy suite (n=1376). We collected information on basic demographics, normal colonoscopies, and histopathology of tissue and polyps removed. Histopathology was divided into groups as follows: [tubular adenoma, low-grade tubular adenoma], [high-grade tubular adenoma, villous adenoma, tubulovillous adenoma], sessile serrated, sessile serrated with dysplasia, traditional serrated adenoma, and carcinoma.
Results: Using a Fisher’s Exact test, there was no significant difference in the detection of carcinoma- 0.13% (2/1565) prior to, 0.57% (8/1398) during, and 0.29% (4/1376) after the shutdown. There was also no significant difference in the rates of the groups of high-risk polyps that were investigated between the time periods. Overall, there was no significant difference in colon cancer surveillance and diagnosis in the time related to endoscopy suite shutdowns during the Covid-19 pandemic at this institution.
Discussion: This study serves as an example of a large academic institution that maintained similar rates of colorectal cancer screening and diagnosis despite limitations on endoscopic procedures during the Covid-19 pandemic. Further investigation is needed to evaluate the long-term effects of the pandemic on colorectal cancer screening.
Disclosures:
Anupama Ancha indicated no relevant financial relationships.
Alexis Bejcek indicated no relevant financial relationships.
Dania Bairuty indicated no relevant financial relationships.
Kenneth Youens indicated no relevant financial relationships.
Christopher Johnson indicated no relevant financial relationships.
Anupama Ancha, MD1, Alexis Bejcek, MD1, Dania Bairuty, DO1, Kenneth Youens, MD2, Christopher Johnson, MD, PhD1. P0333 - The Impact of the COVID-19 Pandemic on Colorectal Cancer Diagnosis by Screening Endoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
