Sunday Poster Session
Category: Colorectal Cancer Prevention
P0356 - Detection of Gastrointestinal Cancer in Individuals Without Clinical Suspicion of Cancer Using a Multi-Cancer Early Detection Test in the PATHFINDER Study
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Charles H. McDonnell, III, MD
Sutter Health
Sacramento, CA
Presenting Author(s)
Award: Presidential Poster Award
Charles H. McDonnell, MD1, Christina A. DIlaveri, MD2, Margarita Lopatin, MS3, Eric T. Fung, MD, PhD4, Eric A. Klein, MD5, Jordan J.. Karlitz, MD, FACG6
1Sutter Health, Sacramento, CA; 2Mayo Clinic, Rochester, MN; 3GRAIL, LLC, Laguna Niguel, CA; 4GRAIL, LLC, Menlo Park, CA; 5GRAIL, Cleveland, OH; 6GRAIL, LLC, Denver, CO
Introduction: Colorectal cancer (CRC) is the only gastrointestinal (GI) cancer with USPSTF-recommended screening guidelines. Other GI cancer (eg, esophageal, liver) screening guidelines are based on predisposing risk factors; however, not all patients who develop cancer would have met the clinical criteria for screening described in the guidelines. A blood-based multi-cancer early detection (MCED) test was evaluated in the prospective PATHFINDER study (NCT04241796; n=6,662). MCED test detection of GI cancers in PATHFINDER is reported here.
Methods: The MCED test uses machine learning to detect cancer-specific methylation patterns in tumor cell-free DNA and predict a cancer signal origin (CSO). Participants in PATHFINDER were age ≥50 years with/without additional cancer risk factors (eg, smoking), not under clinical investigation for cancer, and consented to one year of follow-up surveillance. Participants with a confirmed GI cancer diagnosis were reviewed for cancer signal detected (CSD)/not detected (CSND) result, CSO prediction accuracy, cancer type and stage, and time to diagnostic resolution.
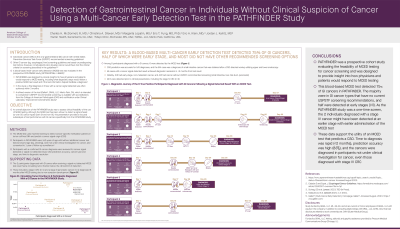
Results: Among 8 participants diagnosed with a GI cancer, 6 were detected by the MCED test (Table 1). CSO prediction was accurate for 5/6 diagnoses, and the sixth case was a diagnosis of small intestine cancer that was obtained after a CSO-directed workup utilizing upper and lower endoscopy. All cases with a CSD result achieved diagnostic resolution in < 2 months from test result. Notably, 3/6 had early-stage, non-metastatic cancer and 4/6 had cancer without USPSTF-recommended screening (small intestine, liver, bile duct, pancreatic). All 6 were detected prior to clinical presentation, including the stage IV CRC (n=2). The 2 participants diagnosed with GI cancer after a CSND result had a circulating tumor fraction below the clinical limit of detection; these include a stage I CRC (n=1) and a stage III pancreatic cancer (n=1) diagnosed 6 months after MCED testing due to new symptom development.
Discussion: This blood-based MCED test detected 75% of GI cancers in PATHFINDER. The majority were in GI cancer types that have no current USPSTF screening recommendations, and half were detected at early stages (I/II). These data support the utility of an MCED test that predicts a CSO as time to diagnosis was rapid (< 2 months), prediction accuracy was high (83%), and the cancers were diagnosed in participants not under clinical investigation for cancer, even those diagnosed with stage IV CRC.
Disclosures:
Charles H. McDonnell, MD1, Christina A. DIlaveri, MD2, Margarita Lopatin, MS3, Eric T. Fung, MD, PhD4, Eric A. Klein, MD5, Jordan J.. Karlitz, MD, FACG6. P0356 - Detection of Gastrointestinal Cancer in Individuals Without Clinical Suspicion of Cancer Using a Multi-Cancer Early Detection Test in the PATHFINDER Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Charles H. McDonnell, MD1, Christina A. DIlaveri, MD2, Margarita Lopatin, MS3, Eric T. Fung, MD, PhD4, Eric A. Klein, MD5, Jordan J.. Karlitz, MD, FACG6
1Sutter Health, Sacramento, CA; 2Mayo Clinic, Rochester, MN; 3GRAIL, LLC, Laguna Niguel, CA; 4GRAIL, LLC, Menlo Park, CA; 5GRAIL, Cleveland, OH; 6GRAIL, LLC, Denver, CO
Introduction: Colorectal cancer (CRC) is the only gastrointestinal (GI) cancer with USPSTF-recommended screening guidelines. Other GI cancer (eg, esophageal, liver) screening guidelines are based on predisposing risk factors; however, not all patients who develop cancer would have met the clinical criteria for screening described in the guidelines. A blood-based multi-cancer early detection (MCED) test was evaluated in the prospective PATHFINDER study (NCT04241796; n=6,662). MCED test detection of GI cancers in PATHFINDER is reported here.
Methods: The MCED test uses machine learning to detect cancer-specific methylation patterns in tumor cell-free DNA and predict a cancer signal origin (CSO). Participants in PATHFINDER were age ≥50 years with/without additional cancer risk factors (eg, smoking), not under clinical investigation for cancer, and consented to one year of follow-up surveillance. Participants with a confirmed GI cancer diagnosis were reviewed for cancer signal detected (CSD)/not detected (CSND) result, CSO prediction accuracy, cancer type and stage, and time to diagnostic resolution.
Results: Among 8 participants diagnosed with a GI cancer, 6 were detected by the MCED test (Table 1). CSO prediction was accurate for 5/6 diagnoses, and the sixth case was a diagnosis of small intestine cancer that was obtained after a CSO-directed workup utilizing upper and lower endoscopy. All cases with a CSD result achieved diagnostic resolution in < 2 months from test result. Notably, 3/6 had early-stage, non-metastatic cancer and 4/6 had cancer without USPSTF-recommended screening (small intestine, liver, bile duct, pancreatic). All 6 were detected prior to clinical presentation, including the stage IV CRC (n=2). The 2 participants diagnosed with GI cancer after a CSND result had a circulating tumor fraction below the clinical limit of detection; these include a stage I CRC (n=1) and a stage III pancreatic cancer (n=1) diagnosed 6 months after MCED testing due to new symptom development.
Discussion: This blood-based MCED test detected 75% of GI cancers in PATHFINDER. The majority were in GI cancer types that have no current USPSTF screening recommendations, and half were detected at early stages (I/II). These data support the utility of an MCED test that predicts a CSO as time to diagnosis was rapid (< 2 months), prediction accuracy was high (83%), and the cancers were diagnosed in participants not under clinical investigation for cancer, even those diagnosed with stage IV CRC.
Table: Gastrointestinal cancer cases in the PATHFINDER study with a cancer signal detected result.
CSO = cancer signal origin; d = days; F = female; m = male; y = years.
CSO = cancer signal origin; d = days; F = female; m = male; y = years.
Disclosures:
Charles McDonnell: Grail – Consultant.
Christina DIlaveri indicated no relevant financial relationships.
Margarita Lopatin: GRAIL – Employee.
Eric Fung: GRAIL, LLC – Employee, Stock-publicly held company(excluding mutual/index funds).
Eric Klein: GRAIL – Employee.
Jordan Karlitz: GastroGirl/GI OnDEMAND – Consultant, Owner/Ownership Interest. GRAIL – Employee.
Charles H. McDonnell, MD1, Christina A. DIlaveri, MD2, Margarita Lopatin, MS3, Eric T. Fung, MD, PhD4, Eric A. Klein, MD5, Jordan J.. Karlitz, MD, FACG6. P0356 - Detection of Gastrointestinal Cancer in Individuals Without Clinical Suspicion of Cancer Using a Multi-Cancer Early Detection Test in the PATHFINDER Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

