Sunday Poster Session
Category: Colorectal Cancer Prevention
P0371 - Not Just a Board Question: Gardner Syndrome in Clinical Practice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Patrick Tempera, DO
Albany Medical Center
Albany, NY
Presenting Author(s)
Patrick Tempera, DO1, Arun Mathew, MD2
1Albany Medical Center, Albany, NY; 2Advanced Gastroenterology Group, Union, NJ
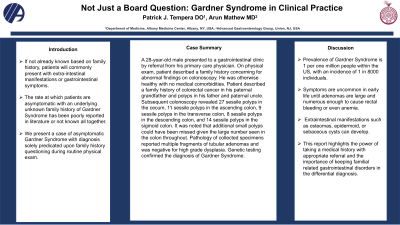
Introduction: The prevalence of Gardner Syndrome within the United States is rare. If not already known based on family history, patients will commonly present with extra-intestinal manifestations or gastrointestinal symptoms. The rate at which patients are asymptomatic with an underlying unknown family history of Gardner Syndrome has been poorly reported in literature or not known all together. We present a case of asymptomatic Gardner Syndrome with diagnosis solely predicated upon family history questioning during routine physical exam.
Case Description/Methods: A 28-year-old male presented to a gastrointestinal clinic by referral from his primary care physician. On physical exam, patient described a family history concerning for abnormal findings on colonoscopy. He was otherwise healthy with no medical comorbidities. Patient described a family history of colorectal cancer in his paternal grandfather and polyps in his father and paternal uncle. Subsequent colonoscopy revealed 27 sessile polyps in the cecum, 11 sessile polyps in the ascending colon, 9 sessile polyps in the transverse colon, 8 sessile polyps in the descending colon, and 14 sessile polyps in the sigmoid colon. It was noted that additional small polyps could have been missed given the large number seen in the colon throughout. Pathology of collected specimens reported multiple fragments of tubular adenomas and was negative for high grade dysplasia. Genetic testing confirmed the diagnosis of Gardner Syndrome.
Discussion: The prevalence of Gardner Syndrome is 1 per one million people within the US, with an incidence of 1 in 8000 individuals. Symptoms are uncommon in early life until adenomas are large and numerous enough to cause rectal bleeding or even anemia. Other non-specific complaints such as change in bowel habits, abdominal pains, or weight loss can lead to further assessment and identification. Extraintestinal manifestations such as osteomas, epidermoid, or sebaceous cysts can develop. However, our patient did not have abdominal complaints, extra-intestinal manifestation, or diagnosed family history. The identification of a colonic genetic disorder such as Gardner Syndrome could have easily gone unnoticed for some time. This report highlights the power of taking a medical history with appropriate referral and the importance of keeping familial related gastrointestinal disorders in the differential diagnosis. Further analyzation is needed regarding under-diagnosed cases of Gardner Syndrome to better understand how to prevent missed cases.
Disclosures:
Patrick Tempera, DO1, Arun Mathew, MD2. P0371 - Not Just a Board Question: Gardner Syndrome in Clinical Practice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Albany Medical Center, Albany, NY; 2Advanced Gastroenterology Group, Union, NJ
Introduction: The prevalence of Gardner Syndrome within the United States is rare. If not already known based on family history, patients will commonly present with extra-intestinal manifestations or gastrointestinal symptoms. The rate at which patients are asymptomatic with an underlying unknown family history of Gardner Syndrome has been poorly reported in literature or not known all together. We present a case of asymptomatic Gardner Syndrome with diagnosis solely predicated upon family history questioning during routine physical exam.
Case Description/Methods: A 28-year-old male presented to a gastrointestinal clinic by referral from his primary care physician. On physical exam, patient described a family history concerning for abnormal findings on colonoscopy. He was otherwise healthy with no medical comorbidities. Patient described a family history of colorectal cancer in his paternal grandfather and polyps in his father and paternal uncle. Subsequent colonoscopy revealed 27 sessile polyps in the cecum, 11 sessile polyps in the ascending colon, 9 sessile polyps in the transverse colon, 8 sessile polyps in the descending colon, and 14 sessile polyps in the sigmoid colon. It was noted that additional small polyps could have been missed given the large number seen in the colon throughout. Pathology of collected specimens reported multiple fragments of tubular adenomas and was negative for high grade dysplasia. Genetic testing confirmed the diagnosis of Gardner Syndrome.
Discussion: The prevalence of Gardner Syndrome is 1 per one million people within the US, with an incidence of 1 in 8000 individuals. Symptoms are uncommon in early life until adenomas are large and numerous enough to cause rectal bleeding or even anemia. Other non-specific complaints such as change in bowel habits, abdominal pains, or weight loss can lead to further assessment and identification. Extraintestinal manifestations such as osteomas, epidermoid, or sebaceous cysts can develop. However, our patient did not have abdominal complaints, extra-intestinal manifestation, or diagnosed family history. The identification of a colonic genetic disorder such as Gardner Syndrome could have easily gone unnoticed for some time. This report highlights the power of taking a medical history with appropriate referral and the importance of keeping familial related gastrointestinal disorders in the differential diagnosis. Further analyzation is needed regarding under-diagnosed cases of Gardner Syndrome to better understand how to prevent missed cases.
Disclosures:
Patrick Tempera indicated no relevant financial relationships.
Arun Mathew indicated no relevant financial relationships.
Patrick Tempera, DO1, Arun Mathew, MD2. P0371 - Not Just a Board Question: Gardner Syndrome in Clinical Practice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
