Sunday Poster Session
Category: Endoscopy Video Forum
P0382 - A Case of EUS Double Bypass
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Deepak K. Johnson, MD, DM
BCMCH
Thiruvalla, Kerala, India
Presenting Author(s)
Deepak K. Johnson, MD, DM
BCMCH, Thiruvalla, Kerala, India
Introduction: Combined biliary + duodenal obstruction due to pancreatic cancer is traditionally managed by Surgical by pass or a combination of ERCP with duodenal SEMS placement.
Case Description/Methods: A 59 year old female presented with abdominal pain, recurrent vomiting and jaundice. Contrast CT scan demonstrated a 4 cm pancreatic head mass with multiple liver metastasis, duodenal and biliary obstruction. An EUS FNB (done from antrum of stomach ) demonstrated adenocarcinoma. ERCP couldn’t be done due tumor infiltration of D1-D2 junction and persistent bleed from site of tumor infiltration. Choledochoduodenostomy wasn’t possible as there was very minimal room in first portion of Duodenum as well. Hence EUS Gastro jejunostomy along with EUS Gall bladder drainage from stomach was planned after ensuring patency of cystic duct by MRCP.
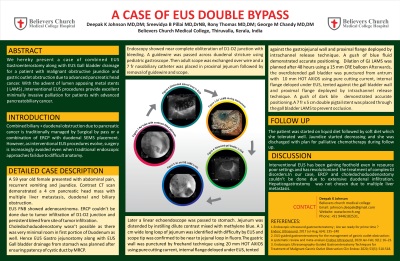
Endoscopy showed near complete obliteration of D1-D2 junction with bleeding. A guidwire was passed across duodenal stricture using pediatric gastroscope .Then adult scope was exchanged over wire and a 7 fr nasobiliary catheter was placed in proximal jejunum followed by removal of guidewire and scope. Later a linear echoendoscope was passed to stomach. Jejunum was distended by instilling dilute contrast mixed with methylene blue. A 3 cm wide long loop of jejunum was identified with difficulty by EUS and scope tip was confirmed to be near to jejunal loop in fluoro. The gastric wall was punctured by freehand technique using 20 mm HOT AXIOS using pure cutting current, internal flange deloyed under EUS, tented against the gastojejunal wall and proximal flange deployed by intrachannel release technique. A gush of blue fluid demonstrated accurate positioning. Dilation of GJ LAMS was planned after 48 hours using a 15 mm CRE balloon.
Afterwards, the overdistended gall bladder was identified by EUS from antrum. The gastric wall was punctured using 10 mm HOT AXIOS using pure cutting current, internal flange deloyed under EUS, tented against the wall and proximal flange deployed by intrachannel release technique. A gush of dark bile demonstrated accurate positioning.A 7 fr x 5 cm double pigtail stent was placed through the gall bladder LAMS to prevent occlusion.
Discussion: Interventional EUS has been gaining foothold even in in resource poor settings and has revolutionized the treatment of complex GI disorders. In our case, ERCP and choledochoduodenostomy couldn’t be done due to extensive duodenal infiltration. Hepaticogastrostomy was not chosen due to multiple liver metastasis.
Disclosures:
Deepak K. Johnson, MD, DM. P0382 - A Case of EUS Double Bypass, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
BCMCH, Thiruvalla, Kerala, India
Introduction: Combined biliary + duodenal obstruction due to pancreatic cancer is traditionally managed by Surgical by pass or a combination of ERCP with duodenal SEMS placement.
Case Description/Methods: A 59 year old female presented with abdominal pain, recurrent vomiting and jaundice. Contrast CT scan demonstrated a 4 cm pancreatic head mass with multiple liver metastasis, duodenal and biliary obstruction. An EUS FNB (done from antrum of stomach ) demonstrated adenocarcinoma. ERCP couldn’t be done due tumor infiltration of D1-D2 junction and persistent bleed from site of tumor infiltration. Choledochoduodenostomy wasn’t possible as there was very minimal room in first portion of Duodenum as well. Hence EUS Gastro jejunostomy along with EUS Gall bladder drainage from stomach was planned after ensuring patency of cystic duct by MRCP.
Endoscopy showed near complete obliteration of D1-D2 junction with bleeding. A guidwire was passed across duodenal stricture using pediatric gastroscope .Then adult scope was exchanged over wire and a 7 fr nasobiliary catheter was placed in proximal jejunum followed by removal of guidewire and scope. Later a linear echoendoscope was passed to stomach. Jejunum was distended by instilling dilute contrast mixed with methylene blue. A 3 cm wide long loop of jejunum was identified with difficulty by EUS and scope tip was confirmed to be near to jejunal loop in fluoro. The gastric wall was punctured by freehand technique using 20 mm HOT AXIOS using pure cutting current, internal flange deloyed under EUS, tented against the gastojejunal wall and proximal flange deployed by intrachannel release technique. A gush of blue fluid demonstrated accurate positioning. Dilation of GJ LAMS was planned after 48 hours using a 15 mm CRE balloon.
Afterwards, the overdistended gall bladder was identified by EUS from antrum. The gastric wall was punctured using 10 mm HOT AXIOS using pure cutting current, internal flange deloyed under EUS, tented against the wall and proximal flange deployed by intrachannel release technique. A gush of dark bile demonstrated accurate positioning.A 7 fr x 5 cm double pigtail stent was placed through the gall bladder LAMS to prevent occlusion.
Discussion: Interventional EUS has been gaining foothold even in in resource poor settings and has revolutionized the treatment of complex GI disorders. In our case, ERCP and choledochoduodenostomy couldn’t be done due to extensive duodenal infiltration. Hepaticogastrostomy was not chosen due to multiple liver metastasis.
Disclosures:
Deepak Johnson indicated no relevant financial relationships.
Deepak K. Johnson, MD, DM. P0382 - A Case of EUS Double Bypass, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
