Sunday Poster Session
Category: Esophagus
P0398 - Vitamin D Levels as a Potential Modifier of Eosinophilic Esophagitis Severity in Adults
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Brenderia A. Cameron, MS
University of North Carolina School of Medicine
Chapel Hill, NC
Presenting Author(s)
Brenderia A.. Cameron, MS1, Carlton W.. Anderon, BS1, Elizabeth T.. Jensen, MPH, PhD2, Evan S. Dellon, MD, MPH1
1University of North Carolina School of Medicine, Chapel Hill, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Factors contributing to the rise in prevalence and heterogeneity of eosinophilic esophagitis (EoE), remain unclear. Low vitamin D has been associated with atopy, but has not been extensively assessed as a modifiable risk factor in EoE. We aimed to assess if serum vitamin D levels in newly diagnosed EoE patients are lower than in non-EoE controls, and examine serum vitamin D levels in relation to features of EoE disease severity.
Methods: This secondary analysis of a prospective cohort study used data and biosamples from adults in the UNC EoE Patient Registry and Biobank. Cases of EoE were defined by consensus guidelines. Controls underwent EGD to evaluate upper GI symptoms and did not have EoE. Prior to each procedure, a blood sample was obtained and stored at -80oC. For this analysis, serum was thawed and 25-hydroxy-vitamin D3 (25-OH-D3) was measured by ELISA (R&D; RDKAP1971). Levels of 25-OH-D3 for cases and controls were compared at baseline. Within cases, levels were compared for clinical, endoscopic, and histologic measures of disease activity.
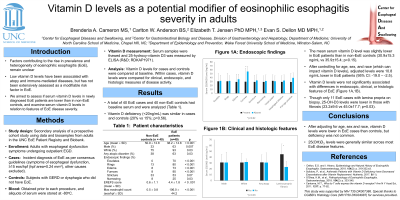
Results: We analyzed 40 EoE cases (mean (SD) age 38.2 (14.8) years; 63% male; 93% white; 63% with any atopic condition; 100% dysphagia) and 40 controls (mean age 50.9 (12.8) years; 33% male; 75% white; 38% with any atopic condition; 90% dysphagia). The mean serum 25-OH-D3 level was slightly lower in EoE patients than in non-EoE controls (30.9 (15.3) ng/mL vs 35.9 (15.4); p=0.15). However, after controlling for age, sex, and race (all of which can impact vitamin D), adjusted levels were 9.0 ng/mL lower in EoE patients (95% CI: -17.1, -1.0; p=0.03). However, 25-OH-D3 deficiency (< 20ng/mL) was similar in cases and controls (20% vs 15%; p=0.56). Levels of 25-OH-D3 were not significantly associated clinical or endoscopic features of EoE (Figure 1), and total EREFS and peak eosinophil counts did not significantly correlate with 25-OH-D3 levels (R of -0.28 [p=0.08] and -0.01 [p=0.93], respectively). Though there were only 11 EoE cases with lamina propria present on biopsy, 25-OH-D3 levels were lower in those with fibrosis (23.2±9.6 vs 45.0±17.7; p=0.03).
Discussion: After adjusting for age, sex, and race, 25-OH-D3 levels were lower in EoE cases than controls, but deficiency was not common. Levels of 25-OH-D3 were generally similar across disease features within EoE cases, with the possible exception of lamina propria fibrosis, indicating that vitamin D may not have a strong role in EoE pathogenesis.

Disclosures:
Brenderia A.. Cameron, MS1, Carlton W.. Anderon, BS1, Elizabeth T.. Jensen, MPH, PhD2, Evan S. Dellon, MD, MPH1. P0398 - Vitamin D Levels as a Potential Modifier of Eosinophilic Esophagitis Severity in Adults, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of North Carolina School of Medicine, Chapel Hill, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Factors contributing to the rise in prevalence and heterogeneity of eosinophilic esophagitis (EoE), remain unclear. Low vitamin D has been associated with atopy, but has not been extensively assessed as a modifiable risk factor in EoE. We aimed to assess if serum vitamin D levels in newly diagnosed EoE patients are lower than in non-EoE controls, and examine serum vitamin D levels in relation to features of EoE disease severity.
Methods: This secondary analysis of a prospective cohort study used data and biosamples from adults in the UNC EoE Patient Registry and Biobank. Cases of EoE were defined by consensus guidelines. Controls underwent EGD to evaluate upper GI symptoms and did not have EoE. Prior to each procedure, a blood sample was obtained and stored at -80oC. For this analysis, serum was thawed and 25-hydroxy-vitamin D3 (25-OH-D3) was measured by ELISA (R&D; RDKAP1971). Levels of 25-OH-D3 for cases and controls were compared at baseline. Within cases, levels were compared for clinical, endoscopic, and histologic measures of disease activity.
Results: We analyzed 40 EoE cases (mean (SD) age 38.2 (14.8) years; 63% male; 93% white; 63% with any atopic condition; 100% dysphagia) and 40 controls (mean age 50.9 (12.8) years; 33% male; 75% white; 38% with any atopic condition; 90% dysphagia). The mean serum 25-OH-D3 level was slightly lower in EoE patients than in non-EoE controls (30.9 (15.3) ng/mL vs 35.9 (15.4); p=0.15). However, after controlling for age, sex, and race (all of which can impact vitamin D), adjusted levels were 9.0 ng/mL lower in EoE patients (95% CI: -17.1, -1.0; p=0.03). However, 25-OH-D3 deficiency (< 20ng/mL) was similar in cases and controls (20% vs 15%; p=0.56). Levels of 25-OH-D3 were not significantly associated clinical or endoscopic features of EoE (Figure 1), and total EREFS and peak eosinophil counts did not significantly correlate with 25-OH-D3 levels (R of -0.28 [p=0.08] and -0.01 [p=0.93], respectively). Though there were only 11 EoE cases with lamina propria present on biopsy, 25-OH-D3 levels were lower in those with fibrosis (23.2±9.6 vs 45.0±17.7; p=0.03).
Discussion: After adjusting for age, sex, and race, 25-OH-D3 levels were lower in EoE cases than controls, but deficiency was not common. Levels of 25-OH-D3 were generally similar across disease features within EoE cases, with the possible exception of lamina propria fibrosis, indicating that vitamin D may not have a strong role in EoE pathogenesis.

Figure: Figure 1
Disclosures:
Brenderia Cameron indicated no relevant financial relationships.
Carlton Anderon indicated no relevant financial relationships.
Elizabeth Jensen: Jazz Pharmaceuticals – Consultant. Regeneron – Consultant. TARGET-GASTRO – Grant/Research Support.
Evan Dellon: Abbott – Consultant. Abbvie – Consultant. Adare/Ellodi – Consultant, Grant/Research Support. Aimmune – Consultant. Akesobio – Consultant. Alfasigma – Consultant. ALK – Consultant. Allakos – Consultant, Grant/Research Support. Amgen – Consultant. Aqilion – Consultant. Arena/Pfizer – Consultant, Grant/Research Support. Aslan – Consultant. AstraZeneca – Consultant, Grant/Research Support. Avir – Consultant. Banner Pharmaceuticals – Grant/Research Support. Biorasi – Consultant. Calypso – Consultant. Celgene/Receptos/BMS – Consultant, Grant/Research Support. Celldex – Consultant. Eli Lilly – Consultant. EsoCap – Consultant. Eupraxia – Consultant. Ferring – Consultant. Gossamer Bio – Consultant. GSK – Consultant, Grant/Research Support. Holoclara – Consultant, Grant/Research Support. Invea – Consultant, Grant/Research Support. Knightpoint – Consultant. Landos – Consultant. LucidDx – Consultant. Meritage – Grant/Research Support. Miraca – Grant/Research Support. Morphic – Consultant. Nexstone Immunology – Consultant. Nutricia – Consultant, Grant/Research Support. Parexel/Calyx – Consultant. Phathom – Consultant. Regeneron Pharmaceuticals Inc. – Consultant, Grant/Research Support. Revolo Biotherapeutics – Consultant, Grant/Research Support. Robarts/Alimentiv – Consultant. Salix – Consultant. Sanofi – Consultant. Shire/Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Upstream Bio – Consultant.
Brenderia A.. Cameron, MS1, Carlton W.. Anderon, BS1, Elizabeth T.. Jensen, MPH, PhD2, Evan S. Dellon, MD, MPH1. P0398 - Vitamin D Levels as a Potential Modifier of Eosinophilic Esophagitis Severity in Adults, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
