Sunday Poster Session
Category: Esophagus
P0402 - Impact of Aspirin Use on Metastasis in Patients With Esophageal Cancer: A Nationwide Analysis 2016-2020
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- JP
Jay Patel, MD
Orange Park Medical Center
Cleveland, OH
Presenting Author(s)
Jay Patel, MD1, Aalam Sohal, MD2, Armaan Dhaliwal, MBBS3, Hunza Chaudhry, MD4, Ishandeep Singh, MBBS5, Shivam Kalra, MBBS6, Dino Dukovic, BS7, Kanwal Bains, MBBS, CNSC3
1Orange Park Medical Center, Jacksonville, FL; 2Liver Institute Northwest, Seattle, WA; 3University of Arizona, Tucson, AZ; 4University of California San Francisco, Fresno, CA; 5Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 6Trident Medical Center, Charleston, SC; 7Ross University School of Medicine, Maramar, FL
Introduction: Despite advancing treatment methods, esophageal cancer(EC) maintains a high mortality rate and poor prognosis. Through various mechanisms, aspirin has been suggested to have a chemopreventive effect on EC. However, the long term effect, particularly regarding rate of metastasis, needs to be further elucidated.
Methods: NIS 2016-2020 was used to identify adult patients(age >18 years) with EC using ICD-10 codes. Patients with missing demographics and mortality were excluded. Patients were stratified into two groups based on aspirin use. Data was collected on patient demographics, Elixhauser Comorbidity Index (ECI), and comorbidities (hypertension, chronic pulmonary disease, coronary artery disease (CAD), chronic kidney disease (CKD), congestive heart failure (CHF), coagulopathy, alcohol use, smoking and obesity). The outcomes studied were rates of gastrointestinal(GI) metastasis, non-GI metastasis and lymphoid metastasis. Multivariate logistic regression analysis was performed to evaluate the impact of aspirin use on metastasis, after adjusting for patient demographics, comorbidities and Elixhauser Comorbidity Index (CCI).
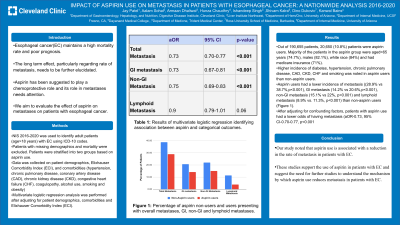
Results: Out of 190,655 patients, 20,650 (10.8%) patients were aspirin users. Majority of the patients in the aspirin group were aged >65 years (74.7%), Males (82.1%), White race (84%) and had medicare insurance (71%). There was a higher incidence of diabetes, hypertension, chronic pulmonary disease, CAD, CKD, CHF and smoking in aspirin users than non-aspirin users. Patients with aspirin users had a lower incidence of GI metastasis (14.2% vs 20.6%,p< 0.001), non-GI metastasis (15.1% vs 22%, p< 0.001) and lymphoid metastasis (8.9% vs. 11.3%, p< 0.001) than non-aspirin users (Figure 1). After adjusting for confounding factors, patients with aspirin use had a lower odds of having GI metastasis (aOR-0.73,95% CI-0.67-0.81, p< 0.001) and non-GI metastasis (aOR-0.75, 95% CI-0.69-0.83, p< 0.001). A trend towards lower odds of lymphoid metastasis (aOR-0.89, 95% CI-0.79-1.01, p< 0.001) was noted in aspirin users (Table 1).
Discussion: Our study noted that aspirin use is associated with a reduction in the rates of both GI and non-GI metastasis in patients with EC. A trend towards reduction in lymphoid metastasis with aspirin use was also noted, but the results were not statistically significant. Further studies examining the mechanism by which aspirin use reduces metastasis in patients with EC are warranted.

Disclosures:
Jay Patel, MD1, Aalam Sohal, MD2, Armaan Dhaliwal, MBBS3, Hunza Chaudhry, MD4, Ishandeep Singh, MBBS5, Shivam Kalra, MBBS6, Dino Dukovic, BS7, Kanwal Bains, MBBS, CNSC3. P0402 - Impact of Aspirin Use on Metastasis in Patients With Esophageal Cancer: A Nationwide Analysis 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Orange Park Medical Center, Jacksonville, FL; 2Liver Institute Northwest, Seattle, WA; 3University of Arizona, Tucson, AZ; 4University of California San Francisco, Fresno, CA; 5Dayanand Medical College and Hospital, Ludhiana, Punjab, India; 6Trident Medical Center, Charleston, SC; 7Ross University School of Medicine, Maramar, FL
Introduction: Despite advancing treatment methods, esophageal cancer(EC) maintains a high mortality rate and poor prognosis. Through various mechanisms, aspirin has been suggested to have a chemopreventive effect on EC. However, the long term effect, particularly regarding rate of metastasis, needs to be further elucidated.
Methods: NIS 2016-2020 was used to identify adult patients(age >18 years) with EC using ICD-10 codes. Patients with missing demographics and mortality were excluded. Patients were stratified into two groups based on aspirin use. Data was collected on patient demographics, Elixhauser Comorbidity Index (ECI), and comorbidities (hypertension, chronic pulmonary disease, coronary artery disease (CAD), chronic kidney disease (CKD), congestive heart failure (CHF), coagulopathy, alcohol use, smoking and obesity). The outcomes studied were rates of gastrointestinal(GI) metastasis, non-GI metastasis and lymphoid metastasis. Multivariate logistic regression analysis was performed to evaluate the impact of aspirin use on metastasis, after adjusting for patient demographics, comorbidities and Elixhauser Comorbidity Index (CCI).
Results: Out of 190,655 patients, 20,650 (10.8%) patients were aspirin users. Majority of the patients in the aspirin group were aged >65 years (74.7%), Males (82.1%), White race (84%) and had medicare insurance (71%). There was a higher incidence of diabetes, hypertension, chronic pulmonary disease, CAD, CKD, CHF and smoking in aspirin users than non-aspirin users. Patients with aspirin users had a lower incidence of GI metastasis (14.2% vs 20.6%,p< 0.001), non-GI metastasis (15.1% vs 22%, p< 0.001) and lymphoid metastasis (8.9% vs. 11.3%, p< 0.001) than non-aspirin users (Figure 1). After adjusting for confounding factors, patients with aspirin use had a lower odds of having GI metastasis (aOR-0.73,95% CI-0.67-0.81, p< 0.001) and non-GI metastasis (aOR-0.75, 95% CI-0.69-0.83, p< 0.001). A trend towards lower odds of lymphoid metastasis (aOR-0.89, 95% CI-0.79-1.01, p< 0.001) was noted in aspirin users (Table 1).
Discussion: Our study noted that aspirin use is associated with a reduction in the rates of both GI and non-GI metastasis in patients with EC. A trend towards reduction in lymphoid metastasis with aspirin use was also noted, but the results were not statistically significant. Further studies examining the mechanism by which aspirin use reduces metastasis in patients with EC are warranted.

Figure: Rates of Metastasis in patients with esophageal cancer, stratified by the presence of Aspirin use.
aOR | 95% CI | p-value | |
GI metastasis | 0.73 | 0.67-0.81 | < 0.001 |
Non-GI Metastasis | 0.75 | 0.69-0.83 | < 0.001 |
Lymphoid Metastasis | 0.89 | 0.79-1.01 | 0.06 |
Table: Results of multivariate analysis assessing the association between metastasis and aspirin use, after adjusting for confounding factors.
Disclosures:
Jay Patel indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Armaan Dhaliwal indicated no relevant financial relationships.
Hunza Chaudhry indicated no relevant financial relationships.
Ishandeep Singh indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Dino Dukovic indicated no relevant financial relationships.
Kanwal Bains indicated no relevant financial relationships.
Jay Patel, MD1, Aalam Sohal, MD2, Armaan Dhaliwal, MBBS3, Hunza Chaudhry, MD4, Ishandeep Singh, MBBS5, Shivam Kalra, MBBS6, Dino Dukovic, BS7, Kanwal Bains, MBBS, CNSC3. P0402 - Impact of Aspirin Use on Metastasis in Patients With Esophageal Cancer: A Nationwide Analysis 2016-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
