Sunday Poster Session
Category: Esophagus
P0413 - To Screen or Not to Screen: Missed Opportunities to Screen for Barrett's Esophagus in Patients Diagnosed with Esophageal Adenocarcinoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Phi P. Tran, DO
Baylor Scott & White
Temple, TX
Presenting Author(s)
Phi P. Tran, DO1, Matthew Tjahja, MD, MS1, Anupama Ancha, MD2, Mark Shell, DO1, Christopher Naumann, DO2
1Baylor Scott & White, Temple, TX; 2Baylor Scott & White Medical Center, Temple, TX
Introduction: The efficacy of Barrett’s Esophagus (BE) and Esophageal Adenocarcinoma (EAC) screening in the general population remains scarce. Screening guidelines remain controversial even for high-risk populations. Our study focused on patients diagnosed with EAC that did not receive screening for BE despite risk factors or did not receive proper BE surveillance. Of these patients, we evaluated the relationship between missed screening opportunities and cancer staging
Methods: Through retrospective chart review of patients with EAC between 2016-2022, age at EAC diagnosis, gender, race, BMI, smoking status and history of GERD and BE were recorded. Initial EGD indication, histologic presence of BE, dysplasia status, and evidence of EAC were identified. Year of EAC diagnosis and cancer staging were determined by oncology notes. Adherence to surveillance interval of 3-5 years was recorded for patients with known NDBE. Per ACG guidelines, missed screening opportunities were defined as males with history of GERD, and two of the following: BMI >30, family history of BE/EAC, smoking history, or Caucasian ethnicity. Multiple logistic regressions and data analyses were utilized to evaluate the relationship with BE surveillance adherence, missed screening opportunities, and cancer staging.
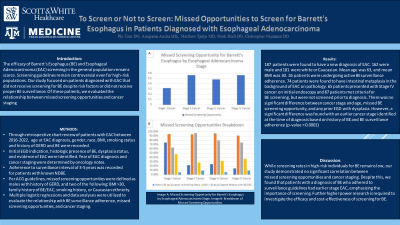
Results: 187 patients were found to have a new diagnosis of EAC. 162 were male and 181 were white or Caucasian. Mean age was 63, and mean BMI was 30. 26 patients were undergoing active BE surveillance adherence. 74 patients were found to have intestinal metaplasia in the background of EAC on pathology. 65 patients presented with Stage IV cancer on initial endoscopy and 87 patients met criteria for BE screening, but were not screened prior to diagnosis. There was no significant difference between cancer stage and age, missed BE screening opportunity, and any prior EGD with dysplasia. However, a significant difference was found with an earlier cancer stage identified at the time of diagnosis based on history of BE and BE surveillance adherence (p-value < 0.0001)
Discussion: While screening rates in high-risk individuals for BE remains low, our study demonstrated no significant correlation between missed screening opportunities and cancer staging. Despite this, we found that patients with a diagnosis of BE who adhered to surveillance guidelines had earlier stage EAC, emphasizing the importance of screening. Further higher power research is required to investigate the efficacy and cost-effectiveness of screening for BE.

Disclosures:
Phi P. Tran, DO1, Matthew Tjahja, MD, MS1, Anupama Ancha, MD2, Mark Shell, DO1, Christopher Naumann, DO2. P0413 - To Screen or Not to Screen: Missed Opportunities to Screen for Barrett's Esophagus in Patients Diagnosed with Esophageal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baylor Scott & White, Temple, TX; 2Baylor Scott & White Medical Center, Temple, TX
Introduction: The efficacy of Barrett’s Esophagus (BE) and Esophageal Adenocarcinoma (EAC) screening in the general population remains scarce. Screening guidelines remain controversial even for high-risk populations. Our study focused on patients diagnosed with EAC that did not receive screening for BE despite risk factors or did not receive proper BE surveillance. Of these patients, we evaluated the relationship between missed screening opportunities and cancer staging
Methods: Through retrospective chart review of patients with EAC between 2016-2022, age at EAC diagnosis, gender, race, BMI, smoking status and history of GERD and BE were recorded. Initial EGD indication, histologic presence of BE, dysplasia status, and evidence of EAC were identified. Year of EAC diagnosis and cancer staging were determined by oncology notes. Adherence to surveillance interval of 3-5 years was recorded for patients with known NDBE. Per ACG guidelines, missed screening opportunities were defined as males with history of GERD, and two of the following: BMI >30, family history of BE/EAC, smoking history, or Caucasian ethnicity. Multiple logistic regressions and data analyses were utilized to evaluate the relationship with BE surveillance adherence, missed screening opportunities, and cancer staging.
Results: 187 patients were found to have a new diagnosis of EAC. 162 were male and 181 were white or Caucasian. Mean age was 63, and mean BMI was 30. 26 patients were undergoing active BE surveillance adherence. 74 patients were found to have intestinal metaplasia in the background of EAC on pathology. 65 patients presented with Stage IV cancer on initial endoscopy and 87 patients met criteria for BE screening, but were not screened prior to diagnosis. There was no significant difference between cancer stage and age, missed BE screening opportunity, and any prior EGD with dysplasia. However, a significant difference was found with an earlier cancer stage identified at the time of diagnosis based on history of BE and BE surveillance adherence (p-value < 0.0001)
Discussion: While screening rates in high-risk individuals for BE remains low, our study demonstrated no significant correlation between missed screening opportunities and cancer staging. Despite this, we found that patients with a diagnosis of BE who adhered to surveillance guidelines had earlier stage EAC, emphasizing the importance of screening. Further higher power research is required to investigate the efficacy and cost-effectiveness of screening for BE.

Figure: Image A: Missed Screening Opportunity for Barrett's Esophagus by Esophageal Adenocarcinoma Stage. Image B: Breakdown of Missed Screening Opportunities.
Disclosures:
Phi Tran indicated no relevant financial relationships.
Matthew Tjahja indicated no relevant financial relationships.
Anupama Ancha indicated no relevant financial relationships.
Mark Shell indicated no relevant financial relationships.
Christopher Naumann indicated no relevant financial relationships.
Phi P. Tran, DO1, Matthew Tjahja, MD, MS1, Anupama Ancha, MD2, Mark Shell, DO1, Christopher Naumann, DO2. P0413 - To Screen or Not to Screen: Missed Opportunities to Screen for Barrett's Esophagus in Patients Diagnosed with Esophageal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
