Sunday Poster Session
Category: Esophagus
P0415 - Personalized Pre-Transplant Manometry Allows Timely Post-Transplant Fundoplication Improving Surgical Outcomes in Lung Transplant Patients
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- TZ
Tian Zhang, BS
Vanderbilt University School of Medicine
Nashville, Tennessee
Presenting Author(s)
Tian Zhang, BS1, Muhammad Hashim Hayat, MD2, Elizabeth F. Sun, BS1, Neil Kapil, MD2, James A. Goss, MD2, Matthew Meyers, MD3, Claudio Roberto Tombazzi, MD4, James Slaughter, BS2, Jasmine Carter, MS2, Dhyanesh Patel, MD2, Michael Vaezi, MD, PhD2, Rishi D. Naik, MD, MSCI2
1Vanderbilt University School of Medicine, Nashville, TN; 2Vanderbilt University Medical Center, Nashville, TN; 3University of Colorado, Denver, CO; 4VUMC, Nashville, TN
Introduction: Lung transplants are associated with high morbidity and mortality among solid organ transplants. Risk factors for poor outcomes include gastroesophageal reflux disease (GERD), which is associated with disease progression, and chronic lung allograft dysfunction (CLAD), which leads to progressive graft failure and death. Heterogeneity remains on pre-transplant esophageal testing regarding manometric and reflux testing. Post-operative management is also variable with surgical fundoplication versus enteral tube placement. We hypothesized that a personalized approach based on indication for pre-transplant manometry can help tailor post-operative fundoplication to help prevent mortality and CLAD.
Methods: In a prospective cohort study, all patients who underwent lung transplantation at a single center in 2009-2022 were analyzed. A prospective predictive approach to manometric indications was completed in real-time to identify high risk manometric findings. Time-to-event analyses using Cox proportional hazards were used for the primary outcomes assessed, mortality and CLAD. Results were plotted by Kaplan-Meier curves tested for significance by log-rank tests.
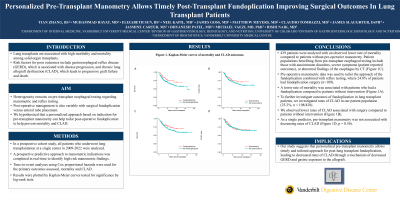
Results: In our study, 439 patients were analyzed with an observed lower rate of mortality compared to patients without pre-operative manometry. Patient populations benefiting from pre-transplant esophageal testing include those with autoimmune disorders, severe symptoms (patient reported outcomes), or abnormal findings of the esophagus by CT (Figure 1C). Pre-operative manometric data was used to tailor the approach of the fundoplication combined with reflux testing, where 24.8% of patients had fundoplication surgery (n=109). A lower rate of mortality was associated with patients who had a fundoplication compared to patients without intervention (Figure 1A). To further investigate outcomes of fundoplication in lung transplant patients, we investigated rates of CLAD in our patient population (25.2%, n = 108/428). We observed lower rates of CLAD associated with surgery compared to patients without intervention (Figure 1B). As a single predictor, pre-transplant manometry was not associated with decreasing rates of CLAD (Figure 1D, p = 0.56).
Discussion: Our study suggests that personalized pre-transplant manometry allows timely and tailored approach for post-lung transplant fundoplication, leading to decreased rates of CLAD through a mechanism of decreased GERD and gastric exposure to the allograft.

Disclosures:
Tian Zhang, BS1, Muhammad Hashim Hayat, MD2, Elizabeth F. Sun, BS1, Neil Kapil, MD2, James A. Goss, MD2, Matthew Meyers, MD3, Claudio Roberto Tombazzi, MD4, James Slaughter, BS2, Jasmine Carter, MS2, Dhyanesh Patel, MD2, Michael Vaezi, MD, PhD2, Rishi D. Naik, MD, MSCI2. P0415 - Personalized Pre-Transplant Manometry Allows Timely Post-Transplant Fundoplication Improving Surgical Outcomes in Lung Transplant Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Vanderbilt University School of Medicine, Nashville, TN; 2Vanderbilt University Medical Center, Nashville, TN; 3University of Colorado, Denver, CO; 4VUMC, Nashville, TN
Introduction: Lung transplants are associated with high morbidity and mortality among solid organ transplants. Risk factors for poor outcomes include gastroesophageal reflux disease (GERD), which is associated with disease progression, and chronic lung allograft dysfunction (CLAD), which leads to progressive graft failure and death. Heterogeneity remains on pre-transplant esophageal testing regarding manometric and reflux testing. Post-operative management is also variable with surgical fundoplication versus enteral tube placement. We hypothesized that a personalized approach based on indication for pre-transplant manometry can help tailor post-operative fundoplication to help prevent mortality and CLAD.
Methods: In a prospective cohort study, all patients who underwent lung transplantation at a single center in 2009-2022 were analyzed. A prospective predictive approach to manometric indications was completed in real-time to identify high risk manometric findings. Time-to-event analyses using Cox proportional hazards were used for the primary outcomes assessed, mortality and CLAD. Results were plotted by Kaplan-Meier curves tested for significance by log-rank tests.
Results: In our study, 439 patients were analyzed with an observed lower rate of mortality compared to patients without pre-operative manometry. Patient populations benefiting from pre-transplant esophageal testing include those with autoimmune disorders, severe symptoms (patient reported outcomes), or abnormal findings of the esophagus by CT (Figure 1C). Pre-operative manometric data was used to tailor the approach of the fundoplication combined with reflux testing, where 24.8% of patients had fundoplication surgery (n=109). A lower rate of mortality was associated with patients who had a fundoplication compared to patients without intervention (Figure 1A). To further investigate outcomes of fundoplication in lung transplant patients, we investigated rates of CLAD in our patient population (25.2%, n = 108/428). We observed lower rates of CLAD associated with surgery compared to patients without intervention (Figure 1B). As a single predictor, pre-transplant manometry was not associated with decreasing rates of CLAD (Figure 1D, p = 0.56).
Discussion: Our study suggests that personalized pre-transplant manometry allows timely and tailored approach for post-lung transplant fundoplication, leading to decreased rates of CLAD through a mechanism of decreased GERD and gastric exposure to the allograft.

Figure: Figure 1. Kaplan-Meier curves of mortality and CLAD outcomes.
Disclosures:
Tian Zhang indicated no relevant financial relationships.
Muhammad Hashim Hayat indicated no relevant financial relationships.
Elizabeth Sun indicated no relevant financial relationships.
Neil Kapil indicated no relevant financial relationships.
James Goss indicated no relevant financial relationships.
Matthew Meyers indicated no relevant financial relationships.
Claudio Roberto Tombazzi indicated no relevant financial relationships.
James Slaughter indicated no relevant financial relationships.
Jasmine Carter indicated no relevant financial relationships.
Dhyanesh Patel indicated no relevant financial relationships.
Michael Vaezi indicated no relevant financial relationships.
Rishi Naik indicated no relevant financial relationships.
Tian Zhang, BS1, Muhammad Hashim Hayat, MD2, Elizabeth F. Sun, BS1, Neil Kapil, MD2, James A. Goss, MD2, Matthew Meyers, MD3, Claudio Roberto Tombazzi, MD4, James Slaughter, BS2, Jasmine Carter, MS2, Dhyanesh Patel, MD2, Michael Vaezi, MD, PhD2, Rishi D. Naik, MD, MSCI2. P0415 - Personalized Pre-Transplant Manometry Allows Timely Post-Transplant Fundoplication Improving Surgical Outcomes in Lung Transplant Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
