Sunday Poster Session
Category: Esophagus
P0456 - Straight from the Stork’s Beak: A Case Series on Achalasia Presenting Postpartum
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Rita Auro, MD
Cooper University Health Care
Camden, NJ
Presenting Author(s)
Rita Auro, MD1, Mary Kathryn Roccato, MD1, Cyrus Mowdawalla, MD2, Daniel Baik, MD1, Joshua DeSipio, MD1
1Cooper University Health Care, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ
Introduction: Achalasia is a Greek term for ‘does not relax’. It involves improper esophageal contraction and impaired lower esophageal sphincter (LES) relaxation. Achalasia during pregnancy is uncommon and is typically diagnosed pre-delivery. However, here we present two unique cases of achalasia presenting postpartum.
Case Description/Methods: A 29-year-old female presented for 3 weeks of dysphagia to solids and liquids with nausea, vomiting, and chest pressure. She had lost 15 pounds after an uncomplicated vaginal delivery 5 weeks prior and was unable to breastfeed due to caloric demands. Due to reflux, she had difficulty tolerating solids during her 3rd trimester but maintained her weight through delivery. Esophagogastroduodenoscopy (EGD) showed mid-distal esophagus distention and a tight LES. Manometry showed a hypersensitive LES with 100% failed swallows and panesophageal pressurization, confirming type II achalasia. After a successful peroral endoscopic myotomy (POEM), her symptoms resolved.
A 31-year-old female presented 10 days postpartum with regurgitation and difficulty swallowing liquids. She had a history of reflux which worsened in her 3rd trimester. After an uncomplicated delivery, she found it impossible to consume solid foods and lost 20 pounds while breastfeeding. Her EGD showed undigested food in the esophagus, which could pass without resistance. Although there was some mucosal variance, biopsies were negative. She underwent a second EGD with dilation one week later due to worsening symptoms. This revealed fluid retention in the esophagus and a tight LES. However, her condition did not improve with dilation. Manometry confirmed the diagnosis of achalasia; following a successful POEM, she reported symptom relief.
Discussion: To our knowledge, there are no documented cases of achalasia presenting postpartum. Both patients suffered from dysphagia to solids during the 3rd trimester, yet symptoms significantly worsened after delivery. While pregnancy increases intragastric pressure, LES resting pressure is physiologically low due to the rise in sex hormones. Progesterone elevation has been shown to decrease smooth muscle tone causing a transient hypotonic LES. Sphincter pressures typically normalize after delivery, yet we theorize the sharp decrease in sex hormones postpartum can lead to an increase in LES pressure, predisposing to achalasia. These cases underscore the need for early postpartum achalasia detection to avert life-threatening maternal and infant malnutrition.

Disclosures:
Rita Auro, MD1, Mary Kathryn Roccato, MD1, Cyrus Mowdawalla, MD2, Daniel Baik, MD1, Joshua DeSipio, MD1. P0456 - Straight from the Stork’s Beak: A Case Series on Achalasia Presenting Postpartum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cooper University Health Care, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ
Introduction: Achalasia is a Greek term for ‘does not relax’. It involves improper esophageal contraction and impaired lower esophageal sphincter (LES) relaxation. Achalasia during pregnancy is uncommon and is typically diagnosed pre-delivery. However, here we present two unique cases of achalasia presenting postpartum.
Case Description/Methods: A 29-year-old female presented for 3 weeks of dysphagia to solids and liquids with nausea, vomiting, and chest pressure. She had lost 15 pounds after an uncomplicated vaginal delivery 5 weeks prior and was unable to breastfeed due to caloric demands. Due to reflux, she had difficulty tolerating solids during her 3rd trimester but maintained her weight through delivery. Esophagogastroduodenoscopy (EGD) showed mid-distal esophagus distention and a tight LES. Manometry showed a hypersensitive LES with 100% failed swallows and panesophageal pressurization, confirming type II achalasia. After a successful peroral endoscopic myotomy (POEM), her symptoms resolved.
A 31-year-old female presented 10 days postpartum with regurgitation and difficulty swallowing liquids. She had a history of reflux which worsened in her 3rd trimester. After an uncomplicated delivery, she found it impossible to consume solid foods and lost 20 pounds while breastfeeding. Her EGD showed undigested food in the esophagus, which could pass without resistance. Although there was some mucosal variance, biopsies were negative. She underwent a second EGD with dilation one week later due to worsening symptoms. This revealed fluid retention in the esophagus and a tight LES. However, her condition did not improve with dilation. Manometry confirmed the diagnosis of achalasia; following a successful POEM, she reported symptom relief.
Discussion: To our knowledge, there are no documented cases of achalasia presenting postpartum. Both patients suffered from dysphagia to solids during the 3rd trimester, yet symptoms significantly worsened after delivery. While pregnancy increases intragastric pressure, LES resting pressure is physiologically low due to the rise in sex hormones. Progesterone elevation has been shown to decrease smooth muscle tone causing a transient hypotonic LES. Sphincter pressures typically normalize after delivery, yet we theorize the sharp decrease in sex hormones postpartum can lead to an increase in LES pressure, predisposing to achalasia. These cases underscore the need for early postpartum achalasia detection to avert life-threatening maternal and infant malnutrition.

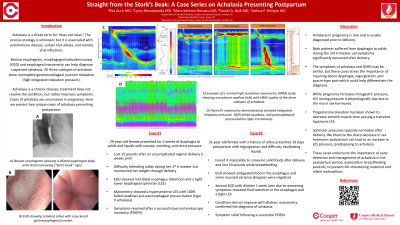
Figure: A. Example of a normal high-resolution manometry (HRM) study showing one patient swallow (left) with HRM studies of the three subtypes of achalasia. B. EGD showing retained saliva with a puckered gastroesophageal junction. C. Barium esophagram showing a dilated esophageal body with distal narrowing (“bird’s beak” sign). D. Patient’s manometry demonstrating elevated integrated relaxation pressure, 100% failed swallows, and panesophageal pressurization (type II achalasia).
Disclosures:
Rita Auro indicated no relevant financial relationships.
Mary Kathryn Roccato indicated no relevant financial relationships.
Cyrus Mowdawalla indicated no relevant financial relationships.
Daniel Baik indicated no relevant financial relationships.
Joshua DeSipio indicated no relevant financial relationships.
Rita Auro, MD1, Mary Kathryn Roccato, MD1, Cyrus Mowdawalla, MD2, Daniel Baik, MD1, Joshua DeSipio, MD1. P0456 - Straight from the Stork’s Beak: A Case Series on Achalasia Presenting Postpartum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

