Sunday Poster Session
Category: Esophagus
P0462 - When Darkness Strikes: Acute Esophageal Necrosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Anumeet S. Tuli, MD
Hamilton Medical Center
Dalton, GA
Presenting Author(s)
Anumeet S. Tuli, MD1, Japjot S. Grewal, MD2, Mohammad Alqaisieh, MD1, Stefan Canacevic, MD3
1Hamilton Medical Center, Dalton, GA; 2Hamilton Health Care System, Dalton, GA; 3Hamilton Medical Center, Chattanooga, TN
Introduction: Acute esophageal necrosis, also referred to as black esophagus or necrotizing esophagitis, is a rare and morbid condition characterized by extensive necrosis and ulceration of the esophageal mucosa. Per an endoscopic series performed in 2004 prevalence ranged from 0.01-0.028% in ten thousand cases1. Although an infrequent entity, it is often seen amongst the critically ill patient population and carries a high mortality. Typical presentation includes upper gastrointestinal bleeding with hematemesis and melena. Despite its high mortality, prompt management is crucial to improve outcomes.
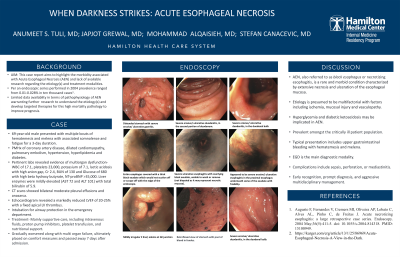
Case Description/Methods: 69-year-old male with a history of CAD, dilated cardiomyopathy, pulmonary embolism, and diabetes presented to the emergency department with multiple bouts of hematemesis and melena with associated somnolence and fatigue for a 3 day duration. The patient was intubated for airway protection in the emergency department. Pertinent labs revealed evidence of multiorgan dysfunction. WBC of 17.1, hemoglobin 13.5, and platelet count of 23,000. In addition, hyperkalemia of 7.1, lactic acidosis with an anion gap of 25, Cr 2.4 with BUN of 130 and Glucose of 680 with high BHB. Liver enzymes were elevated AST 72 and ALT 101 with total bilirubin of 5.9. NT-proBNP > 35,000, troponin gen 5 elevated at 49, negative toxicology. Hepatitis panel, ANA and alpha-1 antitrypsin were negative. CT abdomen/pelvis showed bilateral moderate pleural effusions and anasarca. Echocardiogram revealed LVEF of 20-25% with a fixed apical LV thrombus. EGD demonstrated severe ulcerative and erosive esophagitis with overlying black appearing exudate. This was unable to be washed off, scraped with the edge of endoscope or suctioned – highly concerning for necrotic mucosa. Biopsies of the necrotic tissue were avoided in concern for perforation. No active bleeding was noted. Despite aggressive management the patient continued to develop worsening multi-organ failure.
Discussion: Acute esophageal necrosis remains a rare condition with high mortality rates often associated in critically ill patients. The etiology in our patient is presumed to be multifactorial with contributing factors including ischemia, mucosal injury and vasculopathy. Literature search showed that hyperglycemia and diabetic ketoacidosis may be implicated in AEN in addition to hypoperfusion from hemodynamic instability. EGD remains at the forefront of diagnostic modalities although the underlying mechanism of injury and pathophysiology warrant further research.

Disclosures:
Anumeet S. Tuli, MD1, Japjot S. Grewal, MD2, Mohammad Alqaisieh, MD1, Stefan Canacevic, MD3. P0462 - When Darkness Strikes: Acute Esophageal Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Hamilton Medical Center, Dalton, GA; 2Hamilton Health Care System, Dalton, GA; 3Hamilton Medical Center, Chattanooga, TN
Introduction: Acute esophageal necrosis, also referred to as black esophagus or necrotizing esophagitis, is a rare and morbid condition characterized by extensive necrosis and ulceration of the esophageal mucosa. Per an endoscopic series performed in 2004 prevalence ranged from 0.01-0.028% in ten thousand cases1. Although an infrequent entity, it is often seen amongst the critically ill patient population and carries a high mortality. Typical presentation includes upper gastrointestinal bleeding with hematemesis and melena. Despite its high mortality, prompt management is crucial to improve outcomes.
Case Description/Methods: 69-year-old male with a history of CAD, dilated cardiomyopathy, pulmonary embolism, and diabetes presented to the emergency department with multiple bouts of hematemesis and melena with associated somnolence and fatigue for a 3 day duration. The patient was intubated for airway protection in the emergency department. Pertinent labs revealed evidence of multiorgan dysfunction. WBC of 17.1, hemoglobin 13.5, and platelet count of 23,000. In addition, hyperkalemia of 7.1, lactic acidosis with an anion gap of 25, Cr 2.4 with BUN of 130 and Glucose of 680 with high BHB. Liver enzymes were elevated AST 72 and ALT 101 with total bilirubin of 5.9. NT-proBNP > 35,000, troponin gen 5 elevated at 49, negative toxicology. Hepatitis panel, ANA and alpha-1 antitrypsin were negative. CT abdomen/pelvis showed bilateral moderate pleural effusions and anasarca. Echocardiogram revealed LVEF of 20-25% with a fixed apical LV thrombus. EGD demonstrated severe ulcerative and erosive esophagitis with overlying black appearing exudate. This was unable to be washed off, scraped with the edge of endoscope or suctioned – highly concerning for necrotic mucosa. Biopsies of the necrotic tissue were avoided in concern for perforation. No active bleeding was noted. Despite aggressive management the patient continued to develop worsening multi-organ failure.
Discussion: Acute esophageal necrosis remains a rare condition with high mortality rates often associated in critically ill patients. The etiology in our patient is presumed to be multifactorial with contributing factors including ischemia, mucosal injury and vasculopathy. Literature search showed that hyperglycemia and diabetic ketoacidosis may be implicated in AEN in addition to hypoperfusion from hemodynamic instability. EGD remains at the forefront of diagnostic modalities although the underlying mechanism of injury and pathophysiology warrant further research.

Figure: Esophagoduodenoscopy
A- Proximal esophagus
B- Distal esophagus with GE junction in view
C- Retroflexed view of stomach with pool of blood in fundus.
A- Proximal esophagus
B- Distal esophagus with GE junction in view
C- Retroflexed view of stomach with pool of blood in fundus.
Disclosures:
Anumeet Tuli indicated no relevant financial relationships.
Japjot Grewal indicated no relevant financial relationships.
Mohammad Alqaisieh indicated no relevant financial relationships.
Stefan Canacevic indicated no relevant financial relationships.
Anumeet S. Tuli, MD1, Japjot S. Grewal, MD2, Mohammad Alqaisieh, MD1, Stefan Canacevic, MD3. P0462 - When Darkness Strikes: Acute Esophageal Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
