Sunday Poster Session
Category: Esophagus
P0466 - Don’t Forget the Pemphigus!
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Reyshley Ramos-Marquez, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Reyshley Ramos-Marquez, MD, Carla M. Cepero-Jimenez, MD, Patricia J. Rivera-Cariño, MD, Harry Ruiz-Figueroa, MD, Jose Martin-Ortiz, MD, FACG
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Pemphigus vulgaris (PV) is an autoimmune blistering disorder of the skin and mucosal surfaces which in rare cases can involve esophagus. Affected patients may present with severe dysphagia and odynophagia, and this may result in poor oral intake, weight loss, and malnutrition. We report a case of a patient with PV with esophageal involvement as a cause of dysphagia who required a multidisciplinary approach for diagnosis and treatment.
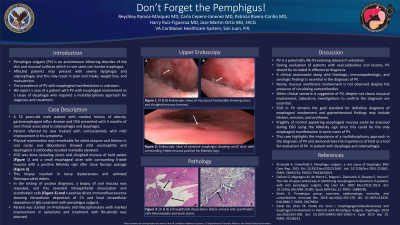
Case Description/Methods: A 53 years-old male patient with medical history of obesity, gastroesophageal reflux disease and OSA presented with 4 months of sore throat associated to odynophagia and dysphagia. Patient referred he was treated with corticosteroids with mild improvement in his symptoms. Physical examination was remarkable for white plaques and blisters in oral cavity. Laboratories showed mild eosinophilia and desmoglein-3 antibodies resulted markedly elevated. Oral blister mucosa was biopsied by Otorhinolaryngology (ENT) service and a small erythematous esophageal ulcer was biopsied by Gastroenterology service and tissue resulted in pathologic findings for non-specific vesico-bullous disorder and loose dyskeratoses and admixed fibrinopurulent debris, respectively. Biopsy of oral mucosa was repeated along with left groin plaque by Dermatology service, and both revealed a positive direct fluorescence, consistent with pemphigus vulgaris. Patient was started on Prednisone with plan of continue with Rituxan.
Discussion: A clinical assessment along with histologic, immunopathologic, and serologic findings is essential in the diagnosis of pemphigus vulgaris. Rarely, mucous membrane involvement is not observed despite the presence of circulating autoantibodies, including desmoglein-3. When clinical scenario is suggestive of PV, despite not classic mucosal involvement, laboratory investigations to confirm the diagnosis are essential. PV tends to be a chronic condition; however, its complications can be life-threatening without treatment. This case highlights the importance of a multidisciplinary approach in the diagnosis of PV and in the setting of negative esophageal biopsies.

Disclosures:
Reyshley Ramos-Marquez, MD, Carla M. Cepero-Jimenez, MD, Patricia J. Rivera-Cariño, MD, Harry Ruiz-Figueroa, MD, Jose Martin-Ortiz, MD, FACG. P0466 - Don’t Forget the Pemphigus!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Pemphigus vulgaris (PV) is an autoimmune blistering disorder of the skin and mucosal surfaces which in rare cases can involve esophagus. Affected patients may present with severe dysphagia and odynophagia, and this may result in poor oral intake, weight loss, and malnutrition. We report a case of a patient with PV with esophageal involvement as a cause of dysphagia who required a multidisciplinary approach for diagnosis and treatment.
Case Description/Methods: A 53 years-old male patient with medical history of obesity, gastroesophageal reflux disease and OSA presented with 4 months of sore throat associated to odynophagia and dysphagia. Patient referred he was treated with corticosteroids with mild improvement in his symptoms. Physical examination was remarkable for white plaques and blisters in oral cavity. Laboratories showed mild eosinophilia and desmoglein-3 antibodies resulted markedly elevated. Oral blister mucosa was biopsied by Otorhinolaryngology (ENT) service and a small erythematous esophageal ulcer was biopsied by Gastroenterology service and tissue resulted in pathologic findings for non-specific vesico-bullous disorder and loose dyskeratoses and admixed fibrinopurulent debris, respectively. Biopsy of oral mucosa was repeated along with left groin plaque by Dermatology service, and both revealed a positive direct fluorescence, consistent with pemphigus vulgaris. Patient was started on Prednisone with plan of continue with Rituxan.
Discussion: A clinical assessment along with histologic, immunopathologic, and serologic findings is essential in the diagnosis of pemphigus vulgaris. Rarely, mucous membrane involvement is not observed despite the presence of circulating autoantibodies, including desmoglein-3. When clinical scenario is suggestive of PV, despite not classic mucosal involvement, laboratory investigations to confirm the diagnosis are essential. PV tends to be a chronic condition; however, its complications can be life-threatening without treatment. This case highlights the importance of a multidisciplinary approach in the diagnosis of PV and in the setting of negative esophageal biopsies.

Figure: Figure 1: (A) Blisters in hard palate (arrow). (B) Esophageal ulcer prior biopsy (arrow).
Disclosures:
Reyshley Ramos-Marquez indicated no relevant financial relationships.
Carla Cepero-Jimenez indicated no relevant financial relationships.
Patricia Rivera-Cariño indicated no relevant financial relationships.
Harry Ruiz-Figueroa indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Reyshley Ramos-Marquez, MD, Carla M. Cepero-Jimenez, MD, Patricia J. Rivera-Cariño, MD, Harry Ruiz-Figueroa, MD, Jose Martin-Ortiz, MD, FACG. P0466 - Don’t Forget the Pemphigus!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
