Sunday Poster Session
Category: Esophagus
P0468 - Pseudotumor Esophagus: An Interesting Culprit of Worsening Odynophagia
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jeremy Polman, DO, MS, MBA
St. David's South Austin Medical Center
New York, NY
Presenting Author(s)
Jeremy Polman, DO, MS, MBA1, Lauren Lyssy, DO2
1St. David's South Austin Medical Center, Nashville, TN; 2St. David's South Austin Medical Center, Austin, TX
Introduction: Odynophagia can be caused by a multitude of pathology, ranging from benign to life threatening. Associated symptoms should be used to direct further evaluation and treatment; however, if patients develop rapidly progressive symptoms or unexpected associated symptoms, prompt evaluation is necessary.
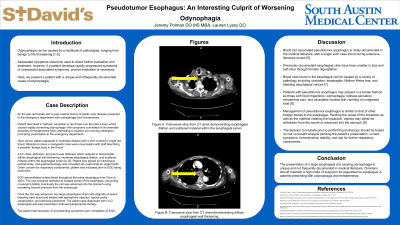
Case Description/Methods: An 83 year-old female with a past medical history of peptic ulcer disease presented to the emergency department with odynophagia and hematemesis. Patient described developing a “fullness” sensation in her throat over the past 4 days, which was caused rapidly worsening odynophagia. Her symptoms culminated in innumerable episodes of hematemesis when attempting to swallow her morning medication, prompting presentation to the emergency department. Upon arrival, patient appeared in moderate distress with a shirt covered in bright red blood. Attempts to place a nasogastric tube were unsuccessful with staff describing a possible “foreign body in the throat.” A CT chest, abdomen, and pelvis was obtained, which seemed to demonstrate diffuse esophageal wall thickening, moderate esophageal dilation, and scattered material within the esophageal lumen. Patient was placed on intravenous pantoprazole, and gastroenterology was consulted who performed an urgent EGD. Given concern for respiratory compromise, patient was intubated prior to EGD being performed. EGD demonstrated what appeared to be clotted blood throughout the entire esophagus, first being encountered at 16cm insertion down to the GE junction at 38cm. The clot seemed to remain adherent at multiple points of the esophagus, preventing movement distally. Eventually the clot was advanced into the stomach using increasing forward pressure from the endoscope. Once the clot was advanced, two large esophageal ulcers with stigmata of recent bleeding were found and treated with epinephrine injection, bipolar probe cauterization, and hemoclip placement. The patient was diagnosed with LA-D esophagitis and was scheduled to receive continued pantoprazole therapy. The patient had resolution of all presenting symptoms upon completion of EGD.
Discussion: The presentation of a large esophageal clot causing odynophagia is unique and not frequently documented in medical literature. Previously documented esophageal clots have been smaller in size and self-clear through forceful regurgitation. Clinicians should maintain a high index of suspicion for pseudotumor esophagus in patients presenting with odynophagia and hematemesis.

Disclosures:
Jeremy Polman, DO, MS, MBA1, Lauren Lyssy, DO2. P0468 - Pseudotumor Esophagus: An Interesting Culprit of Worsening Odynophagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. David's South Austin Medical Center, Nashville, TN; 2St. David's South Austin Medical Center, Austin, TX
Introduction: Odynophagia can be caused by a multitude of pathology, ranging from benign to life threatening. Associated symptoms should be used to direct further evaluation and treatment; however, if patients develop rapidly progressive symptoms or unexpected associated symptoms, prompt evaluation is necessary.
Case Description/Methods: An 83 year-old female with a past medical history of peptic ulcer disease presented to the emergency department with odynophagia and hematemesis. Patient described developing a “fullness” sensation in her throat over the past 4 days, which was caused rapidly worsening odynophagia. Her symptoms culminated in innumerable episodes of hematemesis when attempting to swallow her morning medication, prompting presentation to the emergency department. Upon arrival, patient appeared in moderate distress with a shirt covered in bright red blood. Attempts to place a nasogastric tube were unsuccessful with staff describing a possible “foreign body in the throat.” A CT chest, abdomen, and pelvis was obtained, which seemed to demonstrate diffuse esophageal wall thickening, moderate esophageal dilation, and scattered material within the esophageal lumen. Patient was placed on intravenous pantoprazole, and gastroenterology was consulted who performed an urgent EGD. Given concern for respiratory compromise, patient was intubated prior to EGD being performed. EGD demonstrated what appeared to be clotted blood throughout the entire esophagus, first being encountered at 16cm insertion down to the GE junction at 38cm. The clot seemed to remain adherent at multiple points of the esophagus, preventing movement distally. Eventually the clot was advanced into the stomach using increasing forward pressure from the endoscope. Once the clot was advanced, two large esophageal ulcers with stigmata of recent bleeding were found and treated with epinephrine injection, bipolar probe cauterization, and hemoclip placement. The patient was diagnosed with LA-D esophagitis and was scheduled to receive continued pantoprazole therapy. The patient had resolution of all presenting symptoms upon completion of EGD.
Discussion: The presentation of a large esophageal clot causing odynophagia is unique and not frequently documented in medical literature. Previously documented esophageal clots have been smaller in size and self-clear through forceful regurgitation. Clinicians should maintain a high index of suspicion for pseudotumor esophagus in patients presenting with odynophagia and hematemesis.

Figure: Figures A and B: Anterior-posterior slice from CT angiogram of chest demonstrating esophageal wall thickening and moderate esophageal dilation.
Disclosures:
Jeremy Polman indicated no relevant financial relationships.
Lauren Lyssy indicated no relevant financial relationships.
Jeremy Polman, DO, MS, MBA1, Lauren Lyssy, DO2. P0468 - Pseudotumor Esophagus: An Interesting Culprit of Worsening Odynophagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
