Sunday Poster Session
Category: Esophagus
P0472 - An Unusual Case of Achalasia
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- ST
Suchi Thakker, MD
Montefiore Medical Center/Albert Einstein College of Medicine
Bronx, New York
Presenting Author(s)
Suchi Thakker, MD1, Sherrie White, MD2, Sunny Patel, MD3, Donald P.. Kotler, MD2
1Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY; 2Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY; 3Albert Einstein College of Medicine, Bronx, NY
Introduction: Malnutrition and parasitic infections are known to be associated. Neurocysticercosis (NCC), caused by the parasite Taenia solium, is a common infection in developing countries that manifests as seizure and headache, but can also cause hydrocephalus leading to nausea and vomiting. We present a case that challenges Occam’s razor - a diagnosis of NCC was made that could explain the patient’s symptoms, but the unfolding of his course gave rise to other etiologies that also contributed to his presentation.
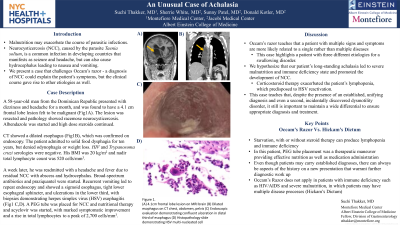
Case Description/Methods: A 58-year-old man from the Dominican Republic presented with dizziness and headache for a month, and was found to have a 4.1 cm frontal lobe lesion felt to be malignant (Fig1A). CT showed a dilated esophagus (Fig1B), which was confirmed on endoscopy. The lesion was resected and pathology showed racemose neurocysticercosis. Albendazole was started, and high dose steroids continued. The patient admitted to solid food dysphagia for ten years, but denied odynophagia or weight loss. HIV and Trypanosoma cruzi serologies were negative. His BMI was 20 kg/m2 and nadir total lymphocyte count was 520 cells/mm3.
A week later, he was readmitted with a headache and fever due to residual NCC with abscess and hydrocephalus. Broad-spectrum antibiotics and praziquantel were started. Recurrent vomiting led to repeat endoscopy and showed a sigmoid esophagus, tight lower esophageal sphincter, and ulcerations in the lower third, with biopsies demonstrating herpes simplex virus (HSV) esophagitis (Fig1C,D). A PEG tube was placed for NCC and nutritional therapies and acyclovir was started, with improvement in symptoms.
Discussion: We hypothesize that our patient’s long-standing achalasia led to malnutrition which caused an immunodeficient state which promoted the development of NCC, which was exacerbated by initiation of steroids as evidenced by an absolute lymphopenia which predisposed to abscess formation and reactivation of HSV. This case highlights a patient with three different etiologies for a swallowing disorder. It teaches that, despite the presence of an established, unifying diagnosis and even a second, incidentally discovered dysmotility disorder, it still is important to maintain a wide differential to ensure appropriate diagnosis and treatment.

Disclosures:
Suchi Thakker, MD1, Sherrie White, MD2, Sunny Patel, MD3, Donald P.. Kotler, MD2. P0472 - An Unusual Case of Achalasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY; 2Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY; 3Albert Einstein College of Medicine, Bronx, NY
Introduction: Malnutrition and parasitic infections are known to be associated. Neurocysticercosis (NCC), caused by the parasite Taenia solium, is a common infection in developing countries that manifests as seizure and headache, but can also cause hydrocephalus leading to nausea and vomiting. We present a case that challenges Occam’s razor - a diagnosis of NCC was made that could explain the patient’s symptoms, but the unfolding of his course gave rise to other etiologies that also contributed to his presentation.
Case Description/Methods: A 58-year-old man from the Dominican Republic presented with dizziness and headache for a month, and was found to have a 4.1 cm frontal lobe lesion felt to be malignant (Fig1A). CT showed a dilated esophagus (Fig1B), which was confirmed on endoscopy. The lesion was resected and pathology showed racemose neurocysticercosis. Albendazole was started, and high dose steroids continued. The patient admitted to solid food dysphagia for ten years, but denied odynophagia or weight loss. HIV and Trypanosoma cruzi serologies were negative. His BMI was 20 kg/m2 and nadir total lymphocyte count was 520 cells/mm3.
A week later, he was readmitted with a headache and fever due to residual NCC with abscess and hydrocephalus. Broad-spectrum antibiotics and praziquantel were started. Recurrent vomiting led to repeat endoscopy and showed a sigmoid esophagus, tight lower esophageal sphincter, and ulcerations in the lower third, with biopsies demonstrating herpes simplex virus (HSV) esophagitis (Fig1C,D). A PEG tube was placed for NCC and nutritional therapies and acyclovir was started, with improvement in symptoms.
Discussion: We hypothesize that our patient’s long-standing achalasia led to malnutrition which caused an immunodeficient state which promoted the development of NCC, which was exacerbated by initiation of steroids as evidenced by an absolute lymphopenia which predisposed to abscess formation and reactivation of HSV. This case highlights a patient with three different etiologies for a swallowing disorder. It teaches that, despite the presence of an established, unifying diagnosis and even a second, incidentally discovered dysmotility disorder, it still is important to maintain a wide differential to ensure appropriate diagnosis and treatment.

Figure: Figure 1. (A) 4.1cm frontal lobe lesion on MRI brain (B) Dilated esophagus on CT chest, abdomen, pelvis (C) Endoscopic evaluation demonstrating confluent ulceration in distal third of esophagus (D) Histopathology slide demonstrating HSV multi-nucleated cell
Disclosures:
Suchi Thakker indicated no relevant financial relationships.
Sherrie White indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Donald Kotler indicated no relevant financial relationships.
Suchi Thakker, MD1, Sherrie White, MD2, Sunny Patel, MD3, Donald P.. Kotler, MD2. P0472 - An Unusual Case of Achalasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
