Sunday Poster Session
Category: Esophagus
P0474 - Ectopic Enigma: Two Cases of Pancreatic Heterotopia in the Esophagus
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Brendan Andres, MD
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Brandon Witten, MD1, Mahek Shahid, MD2, Aws Alameri, MD1, Brendan Andres, MD3, Rolando Leal, MD3, Cameron Thompson, MD3
1University of Arizona-Tucson College of Medicine, Tucson, AZ; 2University of Arizona College of Medicine-Tucson, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ
Introduction: Heterotopic pancreatic tissue in the esophagus is an exceedingly rare finding reported less than 20 times in the literature. Here, we report two cases of esophageal heterotopic pancreatic tissue discovered on EGD at one academic tertiary care center. Our report is unique in that it displays a severe case with a large nodule and an asymptomatic case with a small nodule.
Case Description/Methods: The first patient was a 54-year-old male with past medical history of Nissen fundoplication complicated by severe esophageal dysmotility necessitating G-tube placement, GERD treated mainly with baking soda containing solutions and chronic dyspepsia. Endoscopic evaluation was performed and showed LA Grade B esophagitis, a 3mm mucosal nodule in the lower esophagus, loosened Nissen wrapping, and duodenitis. Esophageal mucosal nodule was biopsied which showed pancreatic heterotopia. Due to the patient's allergies to PPIs/H2 blockers, the patient was counseled to continue an anti-reflux diet, pursue weight loss and explore surgical correction of Nissen.
The second patient was a 64-year old male with a past medical history of chronic GERD exacerbated by exercise. EGD revealed LA grade C reflux esophagitis and short-segment Barrett's esophagus in the lower third of the esophagus. For the Barrett’s esophagus he was started on high dose PPI followed by RFA after no improvement. Surveillance EGD performed six months after their second RFA session showed no visual evidence of Barrett's esophagus. However, it revealed one small nodule present on the edge of the neo-squamous epithelium. Biopsy of the nodule showed squamocolumnar junctional mucosa with pancreatic tissue in the mucosal layer. Decision was made to continue high dose PPI with no additional medical or surgical intervention.
Discussion: Heterotopic pancreatic tissue in the esophagus is usually an incidental finding; however, as in these cases, it has been described in the literature to cause dysphagia, dyspepsia, and GERD. The first patient described significant dysphagia, which may be partially attributed to their lesion and/or the failure of Nissen fundoplication. The second patient’s heterotopic pancreatic tissue caused no symptoms and was revealed in the submucosa after two RFA treatments. Additionally, it is the first case of heterotopic pancreatic tissue in the literature that was subsequently discovered after RFA therapy.

Disclosures:
Brandon Witten, MD1, Mahek Shahid, MD2, Aws Alameri, MD1, Brendan Andres, MD3, Rolando Leal, MD3, Cameron Thompson, MD3. P0474 - Ectopic Enigma: Two Cases of Pancreatic Heterotopia in the Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona-Tucson College of Medicine, Tucson, AZ; 2University of Arizona College of Medicine-Tucson, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ
Introduction: Heterotopic pancreatic tissue in the esophagus is an exceedingly rare finding reported less than 20 times in the literature. Here, we report two cases of esophageal heterotopic pancreatic tissue discovered on EGD at one academic tertiary care center. Our report is unique in that it displays a severe case with a large nodule and an asymptomatic case with a small nodule.
Case Description/Methods: The first patient was a 54-year-old male with past medical history of Nissen fundoplication complicated by severe esophageal dysmotility necessitating G-tube placement, GERD treated mainly with baking soda containing solutions and chronic dyspepsia. Endoscopic evaluation was performed and showed LA Grade B esophagitis, a 3mm mucosal nodule in the lower esophagus, loosened Nissen wrapping, and duodenitis. Esophageal mucosal nodule was biopsied which showed pancreatic heterotopia. Due to the patient's allergies to PPIs/H2 blockers, the patient was counseled to continue an anti-reflux diet, pursue weight loss and explore surgical correction of Nissen.
The second patient was a 64-year old male with a past medical history of chronic GERD exacerbated by exercise. EGD revealed LA grade C reflux esophagitis and short-segment Barrett's esophagus in the lower third of the esophagus. For the Barrett’s esophagus he was started on high dose PPI followed by RFA after no improvement. Surveillance EGD performed six months after their second RFA session showed no visual evidence of Barrett's esophagus. However, it revealed one small nodule present on the edge of the neo-squamous epithelium. Biopsy of the nodule showed squamocolumnar junctional mucosa with pancreatic tissue in the mucosal layer. Decision was made to continue high dose PPI with no additional medical or surgical intervention.
Discussion: Heterotopic pancreatic tissue in the esophagus is usually an incidental finding; however, as in these cases, it has been described in the literature to cause dysphagia, dyspepsia, and GERD. The first patient described significant dysphagia, which may be partially attributed to their lesion and/or the failure of Nissen fundoplication. The second patient’s heterotopic pancreatic tissue caused no symptoms and was revealed in the submucosa after two RFA treatments. Additionally, it is the first case of heterotopic pancreatic tissue in the literature that was subsequently discovered after RFA therapy.

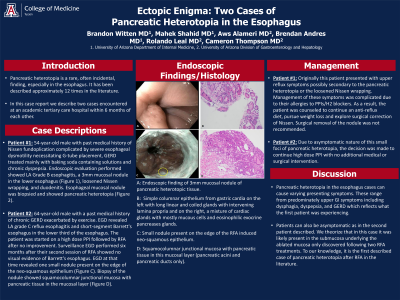
Figure: A: Endoscopic finding of 3mm mucosal nodule of pancreatic heterotopic tissue.
B: Simple columnar epithelium from gastric cardia on the left with long linear and coiled glands with intervening lamina propria and on the right, a mixture of cardiac glands with mostly mucous cells and eosinophilic exocrine pancreases glands.
C: Small nodule present on the edge of the RFA induced neo-squamous epithelium.
D: Squamocolumnar junctional mucosa with pancreatic tissue in this mucosal layer (pancreatic acini and pancreatic ducts only).
B: Simple columnar epithelium from gastric cardia on the left with long linear and coiled glands with intervening lamina propria and on the right, a mixture of cardiac glands with mostly mucous cells and eosinophilic exocrine pancreases glands.
C: Small nodule present on the edge of the RFA induced neo-squamous epithelium.
D: Squamocolumnar junctional mucosa with pancreatic tissue in this mucosal layer (pancreatic acini and pancreatic ducts only).
Disclosures:
Brandon Witten indicated no relevant financial relationships.
Mahek Shahid indicated no relevant financial relationships.
Aws Alameri indicated no relevant financial relationships.
Brendan Andres indicated no relevant financial relationships.
Rolando Leal indicated no relevant financial relationships.
Cameron Thompson indicated no relevant financial relationships.
Brandon Witten, MD1, Mahek Shahid, MD2, Aws Alameri, MD1, Brendan Andres, MD3, Rolando Leal, MD3, Cameron Thompson, MD3. P0474 - Ectopic Enigma: Two Cases of Pancreatic Heterotopia in the Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
