Sunday Poster Session
Category: Esophagus
P0480 - An Unfortunate Case of an Esophagopericardial Fistula
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Phillip Leff, DO
Creighton University
Scottsdale, Arizona
Presenting Author(s)
Phillip Leff, DO1, Austin Saugstad, DO2, Matthew M. Barvo, MD2, Brett A. Dinner, MD2, Robert Lee, MD2, David Tessler, DO3
1Creighton University, Scottsdale, AZ; 2Creighton University, Phoenix, AZ; 3Central Arizona Medical Associates, Mesa, AZ
Introduction: Esophagopericardial fistulas are extraordinarily rare with a fatal prognosis in greater than 50% of patients. Most develop secondary to malignancy or from an injury to the esophagus following surgeries, ablations, or caustic trauma. This case is a grim reminder of the rare potential of esophagopericardial fistula formation, unfortunately found too late on an EGD after an ablation for atrial fibrillation.
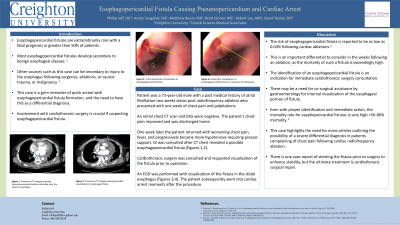
Case Description/Methods: A 73-year-old male with a past medical history of atrial fibrillation two weeks status post radiofrequency ablation presented with one week of chest pain and palpitations. An initial chest CT scan and EKG were negative. Gradually the patient’s chest pain improved and was discharged home. One week later the patient returned with worsening chest pain, fever, and progressively became more hypotensive requiring pressor support. GI was consulted after CT chest (Figures 1,2) revealed a possible esophagopericardial fistula. An initial recommendation to undergo esophagram with gastrografin was not possible due to the patient’s critical condition requiring three pressor support. Cardiothoracic surgery was consulted and requested visualization of the fistula given the high-risk nature of the impending procedure and obscurity of the fistula on the CT scan. An EGD was performed with visualization of the fistula in the distal esophagus (Figures 3,4). The patient subsequently went into cardiac arrest moments after the procedure. The patient was resuscitated though eventually care was withdrawn due to instability and poor prognosis.
Discussion: The risk of esophagopericardial fistula is reported to be as low as 0.04% following cardiac ablations. This complication is an important differential to consider in the weeks following an ablation, as the mortality of such a fistula is exceedingly high. The identification of an esophagopericardial fistula is an indication for immediate cardiothoracic surgery consultation, with possible co-surgical assistance by gastroenterology for internal visualization of the esophageal portion of fistula. This case highlights the need for more articles outlining the possibility of a severe differential diagnosis in patients complaining of chest pain following cardiac radiofrequency ablation. There is one case report of stenting the fistula prior to surgery to enhance stability, but the ultimate treatment is cardiothoracic surgical repair.

Disclosures:
Phillip Leff, DO1, Austin Saugstad, DO2, Matthew M. Barvo, MD2, Brett A. Dinner, MD2, Robert Lee, MD2, David Tessler, DO3. P0480 - An Unfortunate Case of an Esophagopericardial Fistula, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Creighton University, Scottsdale, AZ; 2Creighton University, Phoenix, AZ; 3Central Arizona Medical Associates, Mesa, AZ
Introduction: Esophagopericardial fistulas are extraordinarily rare with a fatal prognosis in greater than 50% of patients. Most develop secondary to malignancy or from an injury to the esophagus following surgeries, ablations, or caustic trauma. This case is a grim reminder of the rare potential of esophagopericardial fistula formation, unfortunately found too late on an EGD after an ablation for atrial fibrillation.
Case Description/Methods: A 73-year-old male with a past medical history of atrial fibrillation two weeks status post radiofrequency ablation presented with one week of chest pain and palpitations. An initial chest CT scan and EKG were negative. Gradually the patient’s chest pain improved and was discharged home. One week later the patient returned with worsening chest pain, fever, and progressively became more hypotensive requiring pressor support. GI was consulted after CT chest (Figures 1,2) revealed a possible esophagopericardial fistula. An initial recommendation to undergo esophagram with gastrografin was not possible due to the patient’s critical condition requiring three pressor support. Cardiothoracic surgery was consulted and requested visualization of the fistula given the high-risk nature of the impending procedure and obscurity of the fistula on the CT scan. An EGD was performed with visualization of the fistula in the distal esophagus (Figures 3,4). The patient subsequently went into cardiac arrest moments after the procedure. The patient was resuscitated though eventually care was withdrawn due to instability and poor prognosis.
Discussion: The risk of esophagopericardial fistula is reported to be as low as 0.04% following cardiac ablations. This complication is an important differential to consider in the weeks following an ablation, as the mortality of such a fistula is exceedingly high. The identification of an esophagopericardial fistula is an indication for immediate cardiothoracic surgery consultation, with possible co-surgical assistance by gastroenterology for internal visualization of the esophageal portion of fistula. This case highlights the need for more articles outlining the possibility of a severe differential diagnosis in patients complaining of chest pain following cardiac radiofrequency ablation. There is one case report of stenting the fistula prior to surgery to enhance stability, but the ultimate treatment is cardiothoracic surgical repair.

Figure: Figures 1,2: CT scans of esophagopericardial fistula
Figures 2,3: Direct visualization of esophagopericardial fistula in the distal esophagus during EGD
Figures 2,3: Direct visualization of esophagopericardial fistula in the distal esophagus during EGD
Disclosures:
Phillip Leff indicated no relevant financial relationships.
Austin Saugstad indicated no relevant financial relationships.
Matthew Barvo indicated no relevant financial relationships.
Brett Dinner indicated no relevant financial relationships.
Robert Lee indicated no relevant financial relationships.
David Tessler indicated no relevant financial relationships.
Phillip Leff, DO1, Austin Saugstad, DO2, Matthew M. Barvo, MD2, Brett A. Dinner, MD2, Robert Lee, MD2, David Tessler, DO3. P0480 - An Unfortunate Case of an Esophagopericardial Fistula, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
