Sunday Poster Session
Category: Esophagus
P0482 - Underdiagnosed Esophageal Lichen Planus: A Stricturing and Precancerous Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- LN
Le Yu Naing, MD
University of Louisville
Louisville, Kentucky
Presenting Author(s)
Le Yu Naing, MD1, Navroop Nagra, MD2, Prateek Mathur, MD1, Dylan Flaherty, DO1, Ali Jaan, MD3, Mohammad Bilal, MD3, Endashaw Omer, MD, MPH, FACG2, Thomas Abell, MD4
1University of Louisville, Louisville, KY; 2University of Louisville School of Medicine, Louisville, KY; 3Rochester General Hospital, Rochester, NY; 4University of Louisville, Louisville, LA
Introduction: Esophageal lichen planus (ELP) is an under-reported and unusual cause of dysphagia in middle- to older-age women. Lichen planus is a chronic mucocutaneous disease affecting the skin, fingernails, and mucosal surfaces. We present a case of dysphagia and odynophagia due to esophageal stricture and ulceration due to ELP.
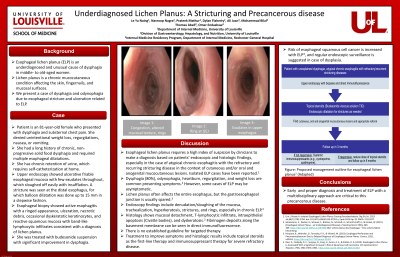
Case Description/Methods: The patient is an 81-year-old female who presented to the emergency department with dysphagia and substernal chest pain. She denied unintentional weight loss, regurgitations, nausea, or vomiting. She had a long history of chronic, non-progressive solid food dysphagia and required multiple esophageal dilatations. Upper endoscopy showed ulcerative friable esophageal mucosa with few exudates throughout, which sloughed off easily with insufflation. A stricture was seen at the distal esophagus, for which balloon dilatation was done up to 15 mm in a stepwise fashion. Esophageal biopsy showed active esophagitis with a ringed appearance, ulceration, necrotic debris, occasional dyskeratotic keratinocytes, and reactive squamous mucosa with band-like lymphocytic infiltrates consistent with a diagnosis of lichen planus. She required self-catheterization at home due to chronic retention of urine with chronic vaginal inflammation due to vaginal lichen planus. She also had oral lichen planus lesions. She was treated with budesonide suspension with significant improvement in dysphagia.
Discussion: Esophageal lichen planus requires a high index of suspicion by clinicians to make a diagnosis based on patients’ endoscopic and histologic findings, especially in the case of atypical chronic esophagitis with the refractory and recurring stricturing disease in the context of cutaneous and/or oral and anogenital mucocutaneous lesions. Lichen planus often affects the entire esophagus, but the gastroesophageal junction is usually spared1, and the proximal and mid-esophagus are involved with the superficial ulceration with exudates and the formation of strictures and rings. There is no established targeted therapy currently. Treatment to improve symptoms and histologic results includes topical steroids as the first-line therapy and immunosuppressant therapy for severe refractory disease. Risk of esophageal cancer is increased with ELP2, and regular endoscopic surveillance is suggested in case of dysplasia. Early diagnosis and treatment with a multidisciplinary approach are critical to this precancerous disease.

Disclosures:
Le Yu Naing, MD1, Navroop Nagra, MD2, Prateek Mathur, MD1, Dylan Flaherty, DO1, Ali Jaan, MD3, Mohammad Bilal, MD3, Endashaw Omer, MD, MPH, FACG2, Thomas Abell, MD4. P0482 - Underdiagnosed Esophageal Lichen Planus: A Stricturing and Precancerous Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Louisville, Louisville, KY; 2University of Louisville School of Medicine, Louisville, KY; 3Rochester General Hospital, Rochester, NY; 4University of Louisville, Louisville, LA
Introduction: Esophageal lichen planus (ELP) is an under-reported and unusual cause of dysphagia in middle- to older-age women. Lichen planus is a chronic mucocutaneous disease affecting the skin, fingernails, and mucosal surfaces. We present a case of dysphagia and odynophagia due to esophageal stricture and ulceration due to ELP.
Case Description/Methods: The patient is an 81-year-old female who presented to the emergency department with dysphagia and substernal chest pain. She denied unintentional weight loss, regurgitations, nausea, or vomiting. She had a long history of chronic, non-progressive solid food dysphagia and required multiple esophageal dilatations. Upper endoscopy showed ulcerative friable esophageal mucosa with few exudates throughout, which sloughed off easily with insufflation. A stricture was seen at the distal esophagus, for which balloon dilatation was done up to 15 mm in a stepwise fashion. Esophageal biopsy showed active esophagitis with a ringed appearance, ulceration, necrotic debris, occasional dyskeratotic keratinocytes, and reactive squamous mucosa with band-like lymphocytic infiltrates consistent with a diagnosis of lichen planus. She required self-catheterization at home due to chronic retention of urine with chronic vaginal inflammation due to vaginal lichen planus. She also had oral lichen planus lesions. She was treated with budesonide suspension with significant improvement in dysphagia.
Discussion: Esophageal lichen planus requires a high index of suspicion by clinicians to make a diagnosis based on patients’ endoscopic and histologic findings, especially in the case of atypical chronic esophagitis with the refractory and recurring stricturing disease in the context of cutaneous and/or oral and anogenital mucocutaneous lesions. Lichen planus often affects the entire esophagus, but the gastroesophageal junction is usually spared1, and the proximal and mid-esophagus are involved with the superficial ulceration with exudates and the formation of strictures and rings. There is no established targeted therapy currently. Treatment to improve symptoms and histologic results includes topical steroids as the first-line therapy and immunosuppressant therapy for severe refractory disease. Risk of esophageal cancer is increased with ELP2, and regular endoscopic surveillance is suggested in case of dysplasia. Early diagnosis and treatment with a multidisciplinary approach are critical to this precancerous disease.

Figure: Esophageal Lichen Planus
Disclosures:
Le Yu Naing indicated no relevant financial relationships.
Navroop Nagra indicated no relevant financial relationships.
Prateek Mathur indicated no relevant financial relationships.
Dylan Flaherty indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Mohammad Bilal indicated no relevant financial relationships.
Endashaw Omer indicated no relevant financial relationships.
Thomas Abell indicated no relevant financial relationships.
Le Yu Naing, MD1, Navroop Nagra, MD2, Prateek Mathur, MD1, Dylan Flaherty, DO1, Ali Jaan, MD3, Mohammad Bilal, MD3, Endashaw Omer, MD, MPH, FACG2, Thomas Abell, MD4. P0482 - Underdiagnosed Esophageal Lichen Planus: A Stricturing and Precancerous Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
