Sunday Poster Session
Category: Esophagus
P0505 - Double-Barrel Esophagus: When All Roads Lead to Dysphagia
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Aaron B. Fein, DO
University of Kentucky
Lexington, KY
Presenting Author(s)
Aaron B. Fein, DO, Cody Kern, MD, Donald Campbell, MD
University of Kentucky, Lexington, KY
Introduction: An esophagogastric fistula, previously termed “double-barrel” esophagus, is an uncommon endoscopic discovery. Esophagogastric fistulas are associated with gastroesophageal reflux disease (GERD), prior esophagogastric surgery, and esophageal carcinoma. Previous esophageal dilations of esophageal strictures have been found to be a predisposing factor in some reported cases. We present a patient with progressive dysphagia and prior stricture dilations who was found to have a distal esophagogastric fistula amenable to endoscopic septotomy.
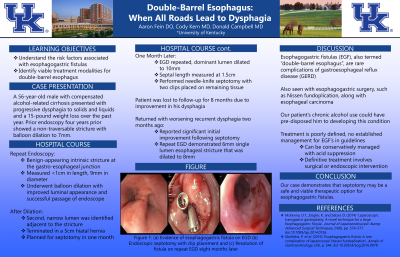
Case Description/Methods: A 56-year-old male with compensated alcohol-related cirrhosis presented with progressive dysphagia to solids and liquids and a 15-pound weight loss over the past year. Previous endoscopy 4 years ago described a non-transversable stricture with balloon dilation to 7mm. Upon esophageal intubation, a benign-appearing intrinsic stricture was identified at the gastro-esophageal (GE) junction, measuring < 1cm in length and 9mm in diameter. He underwent balloon dilation with subsequent improved passage of the scope and luminal appearance. Following dilation, a second, narrow lumen was identified adjacent to the stricture, which appeared to lead to a 5cm hiatal hernia. Repeat endoscopy with planned septotomy was scheduled one month later. Endoscopy re-demonstrated his esophagogastric fistula or “double-barrel” esophagus. The dominant lumen was dilated to 10mm to allow passage of standard gastroscope. The septal length was measured at 1.5cm. Wires were introduced into each lumen to confirm gastric connection. Needle knife septotomy was performed with two clips placed on the remaining tissue. The patient was lost to follow up for 8 months. He re-emerged with recurrent dysphagia over the last 2 months. He reported significant initial improvement after septotomy. Repeat upper endoscopy revealed a single lumen esophageal stricture with 6mm diameter dilated to 8mm with plans for further dilation.
Discussion: Esophagogastric fistula is a rare complication of GERD. This case supports the notion that previous esophageal dilations may predispose their formation. Our patient’s chronic alcohol use may have also contributed. The treatment for these fistulas is poorly defined and not established in the guidelines. They can be conservatively managed with acid suppression, but definitive treatment would rely on surgical or endoscopic intervention. Our case demonstrates that septotmy may be a safe and viable therapeutic option for double barrel esophagus.

Disclosures:
Aaron B. Fein, DO, Cody Kern, MD, Donald Campbell, MD. P0505 - Double-Barrel Esophagus: When All Roads Lead to Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: An esophagogastric fistula, previously termed “double-barrel” esophagus, is an uncommon endoscopic discovery. Esophagogastric fistulas are associated with gastroesophageal reflux disease (GERD), prior esophagogastric surgery, and esophageal carcinoma. Previous esophageal dilations of esophageal strictures have been found to be a predisposing factor in some reported cases. We present a patient with progressive dysphagia and prior stricture dilations who was found to have a distal esophagogastric fistula amenable to endoscopic septotomy.
Case Description/Methods: A 56-year-old male with compensated alcohol-related cirrhosis presented with progressive dysphagia to solids and liquids and a 15-pound weight loss over the past year. Previous endoscopy 4 years ago described a non-transversable stricture with balloon dilation to 7mm. Upon esophageal intubation, a benign-appearing intrinsic stricture was identified at the gastro-esophageal (GE) junction, measuring < 1cm in length and 9mm in diameter. He underwent balloon dilation with subsequent improved passage of the scope and luminal appearance. Following dilation, a second, narrow lumen was identified adjacent to the stricture, which appeared to lead to a 5cm hiatal hernia. Repeat endoscopy with planned septotomy was scheduled one month later. Endoscopy re-demonstrated his esophagogastric fistula or “double-barrel” esophagus. The dominant lumen was dilated to 10mm to allow passage of standard gastroscope. The septal length was measured at 1.5cm. Wires were introduced into each lumen to confirm gastric connection. Needle knife septotomy was performed with two clips placed on the remaining tissue. The patient was lost to follow up for 8 months. He re-emerged with recurrent dysphagia over the last 2 months. He reported significant initial improvement after septotomy. Repeat upper endoscopy revealed a single lumen esophageal stricture with 6mm diameter dilated to 8mm with plans for further dilation.
Discussion: Esophagogastric fistula is a rare complication of GERD. This case supports the notion that previous esophageal dilations may predispose their formation. Our patient’s chronic alcohol use may have also contributed. The treatment for these fistulas is poorly defined and not established in the guidelines. They can be conservatively managed with acid suppression, but definitive treatment would rely on surgical or endoscopic intervention. Our case demonstrates that septotmy may be a safe and viable therapeutic option for double barrel esophagus.

Figure: Figure 1: (a) Evidence of esophagogastric fistula on EGD (b) Endoscopic septotomy with clip placement and (c) Resolution of fistula on repeat EGD eight months later
Disclosures:
Aaron Fein indicated no relevant financial relationships.
Cody Kern indicated no relevant financial relationships.
Donald Campbell indicated no relevant financial relationships.
Aaron B. Fein, DO, Cody Kern, MD, Donald Campbell, MD. P0505 - Double-Barrel Esophagus: When All Roads Lead to Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
