Sunday Poster Session
Category: Esophagus
P0506 - Epidermolysis Bullosa Acquisita With Esophageal Involvement – A Case Report
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Thomas M. Ruli, Jr., MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Thomas M. Ruli, MD, Aditi Jani, MD, MSPH
University of Alabama at Birmingham, Birmingham, AL
Introduction: Epidermolysis Bullosa Acquisita (EBA) is a rare autoimmune disease involving chronic inflammation, blistering and associated scarring of the skin. In rare cases, EBA extends from strictly skin involvement to additional involvement of the mucosal surfaces of the gastrointestinal (GI) tract. Here, we present a case of EBA with esophageal involvement.
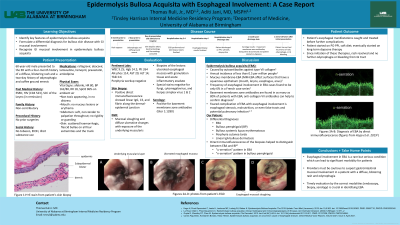
Case Description/Methods: A sixty-year-old male presented to the hospital with a four-month history of a diffuse, blistering rash and a two-day history of odynophagia with coffee ground emesis. On examination, the patient had scattered hemorrhagic and flaccid bullae present on all four extremities as well as on his chest and abdomen. Biopsies of the skin lesions were taken and positive direct immunofluorescence was significant for linear IgG, C3 and fibrin along the dermal-epidermal junction. The patient underwent esophagogastroduodenoscopy (EGD) which showed mucosal sloughing and diffuse ulcerative changes in the proximal and middle third of the esophagus with exposure of the underlying muscularis (figures A-D). Biopsies of the lesions were taken; they revealed ulcerated esophageal mucosa with granulation tissue and acute inflammatory exudate. Special stains were negative for fungi, cytomegalovirus and herpes simplex virus 1 & 2. Serology was significant for positive basement membrane zone antibodies. Immunofluorescence pattern, serology and clinical picture were all most consistent with a diagnosis of EBA with esophageal involvement. The patient was started on oral proton pump inhibitor therapy and eventually placed on long term dapsone therapy. After initiation of these treatments, the patient’s rash resolved and he had no further odynophagia or bleeding from the GI tract.
Discussion: Esophageal involvement in EBA is a rare but nonetheless serious condition which can lead to significant morbidity for patients. One of the most feared complications of this condition is esophageal stenosis; if left untreated it can lead to weight loss, malnutrition or even false tracts and potential pulmonary infection. For our patient, his disease was treated before progression to the prior mentioned complications. Providers must be cautious to suspect GI mucosal involvement in a patient with a diffuse blistering rash and odynophagia.

Disclosures:
Thomas M. Ruli, MD, Aditi Jani, MD, MSPH. P0506 - Epidermolysis Bullosa Acquisita With Esophageal Involvement – A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Alabama at Birmingham, Birmingham, AL
Introduction: Epidermolysis Bullosa Acquisita (EBA) is a rare autoimmune disease involving chronic inflammation, blistering and associated scarring of the skin. In rare cases, EBA extends from strictly skin involvement to additional involvement of the mucosal surfaces of the gastrointestinal (GI) tract. Here, we present a case of EBA with esophageal involvement.
Case Description/Methods: A sixty-year-old male presented to the hospital with a four-month history of a diffuse, blistering rash and a two-day history of odynophagia with coffee ground emesis. On examination, the patient had scattered hemorrhagic and flaccid bullae present on all four extremities as well as on his chest and abdomen. Biopsies of the skin lesions were taken and positive direct immunofluorescence was significant for linear IgG, C3 and fibrin along the dermal-epidermal junction. The patient underwent esophagogastroduodenoscopy (EGD) which showed mucosal sloughing and diffuse ulcerative changes in the proximal and middle third of the esophagus with exposure of the underlying muscularis (figures A-D). Biopsies of the lesions were taken; they revealed ulcerated esophageal mucosa with granulation tissue and acute inflammatory exudate. Special stains were negative for fungi, cytomegalovirus and herpes simplex virus 1 & 2. Serology was significant for positive basement membrane zone antibodies. Immunofluorescence pattern, serology and clinical picture were all most consistent with a diagnosis of EBA with esophageal involvement. The patient was started on oral proton pump inhibitor therapy and eventually placed on long term dapsone therapy. After initiation of these treatments, the patient’s rash resolved and he had no further odynophagia or bleeding from the GI tract.
Discussion: Esophageal involvement in EBA is a rare but nonetheless serious condition which can lead to significant morbidity for patients. One of the most feared complications of this condition is esophageal stenosis; if left untreated it can lead to weight loss, malnutrition or even false tracts and potential pulmonary infection. For our patient, his disease was treated before progression to the prior mentioned complications. Providers must be cautious to suspect GI mucosal involvement in a patient with a diffuse blistering rash and odynophagia.

Figure: A, B: proximal third of the esophagus as seen on patient's EGD
C, D: middle third of the esophagus as seen on patient's EGD
C, D: middle third of the esophagus as seen on patient's EGD
Disclosures:
Thomas Ruli indicated no relevant financial relationships.
Aditi Jani indicated no relevant financial relationships.
Thomas M. Ruli, MD, Aditi Jani, MD, MSPH. P0506 - Epidermolysis Bullosa Acquisita With Esophageal Involvement – A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

