Sunday Poster Session
Category: Esophagus
P0509 - A Case of Rapidly Progressive Severe Dysphagia in a Patient With Dermatomyositis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Khandokar A. Talib, MD
United Health Services Hospital
Vestal, NY
Presenting Author(s)
Khandokar A. Talib, MD1, Khaleeq Siddiqui, MD2, Yasir Ahmed, MD2, Tasnima Elahi, MD3, Leslie Bank, MD2
1United Health Services Hospital, Vestal, NY; 2United Health Services Hospital, Johnson City, NY; 3Stony Brook University, Stony Brook, NY
Introduction: Rapidly progressive severe dysphagia is a rare occurrence associated with Dermatomyositis. It is due to the weakness of the oropharyngeal muscles and the upper one-third of the esophageal muscles.
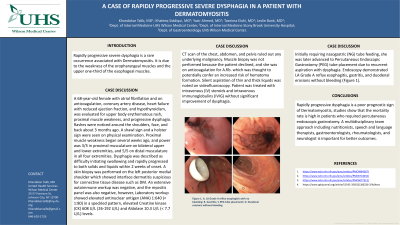
Case Description/Methods: A 68-year-old female with atrial fibrillation and on anticoagulation, coronary artery disease, heart failure with reduced ejection fraction, and hypothyroidism, was evaluated for upper body erythematous rash, proximal muscle weakness, and progressive dysphagia. Rashes were noticed around the shoulders, face, and back about 3 months ago. A shawl sign and a holster sign were seen on physical examination. Proximal muscle weakness began several weeks ago, and power was 3/5 in proximal musculature on bilateral upper and lower extremities, and 5/5 on distal musculature in all four extremities. Dysphagia was described as difficulty initiating swallowing and rapidly progressed to both solids and liquids within 2 weeks of onset. A skin biopsy was performed on the left posterior medial shoulder which showed interface dermatitis suspicious for connective tissue disease such as DM. An extensive autoimmune workup was negative, and the myositis panel was also negative, however, Laboratory workup showed elevated antinuclear antigen (ANA) 1:640 (< 1:80) in a speckled pattern, elevated Creatine kinase (CK) 608 U/L (26-192 U/L) and Aldolase 10.3 U/L (< 7.7 U/L) levels. CT scan of the chest, abdomen, and pelvis ruled out any underlying malignancy. Muscle biopsy was not performed because the patient declined, and she was on anticoagulation for A.fib which was thought to potentially confer an increased risk of hematoma formation. Silent aspiration of thin and thick liquids was noted on videofluoroscopy. Patient was treated with intravenous (IV) steroids and intravenous immunoglobulins (IVIG) without significant improvement of dysphagia. Initially requiring nasogastric (NG) tube feeding, she was later advanced to Percutaneous Endoscopic Gastrostomy (PEG) tube placement due to recurrent aspiration with dysphagia. Endoscopy demonstrated LA Grade A reflux esophagitis, gastritis, and duodenal erosions without bleeding.
Discussion: Rapidly progressive dysphagia is a poor prognostic sign of Dermatomyositis, studies show that the mortality rate is high in patients who required percutaneous endoscopic gastrostomy. A multidisciplinary team approach including nutritionists, speech and language therapists, gastroenterologists, rheumatologists, and neurologist is important for better outcomes.

Disclosures:
Khandokar A. Talib, MD1, Khaleeq Siddiqui, MD2, Yasir Ahmed, MD2, Tasnima Elahi, MD3, Leslie Bank, MD2. P0509 - A Case of Rapidly Progressive Severe Dysphagia in a Patient With Dermatomyositis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1United Health Services Hospital, Vestal, NY; 2United Health Services Hospital, Johnson City, NY; 3Stony Brook University, Stony Brook, NY
Introduction: Rapidly progressive severe dysphagia is a rare occurrence associated with Dermatomyositis. It is due to the weakness of the oropharyngeal muscles and the upper one-third of the esophageal muscles.
Case Description/Methods: A 68-year-old female with atrial fibrillation and on anticoagulation, coronary artery disease, heart failure with reduced ejection fraction, and hypothyroidism, was evaluated for upper body erythematous rash, proximal muscle weakness, and progressive dysphagia. Rashes were noticed around the shoulders, face, and back about 3 months ago. A shawl sign and a holster sign were seen on physical examination. Proximal muscle weakness began several weeks ago, and power was 3/5 in proximal musculature on bilateral upper and lower extremities, and 5/5 on distal musculature in all four extremities. Dysphagia was described as difficulty initiating swallowing and rapidly progressed to both solids and liquids within 2 weeks of onset. A skin biopsy was performed on the left posterior medial shoulder which showed interface dermatitis suspicious for connective tissue disease such as DM. An extensive autoimmune workup was negative, and the myositis panel was also negative, however, Laboratory workup showed elevated antinuclear antigen (ANA) 1:640 (< 1:80) in a speckled pattern, elevated Creatine kinase (CK) 608 U/L (26-192 U/L) and Aldolase 10.3 U/L (< 7.7 U/L) levels. CT scan of the chest, abdomen, and pelvis ruled out any underlying malignancy. Muscle biopsy was not performed because the patient declined, and she was on anticoagulation for A.fib which was thought to potentially confer an increased risk of hematoma formation. Silent aspiration of thin and thick liquids was noted on videofluoroscopy. Patient was treated with intravenous (IV) steroids and intravenous immunoglobulins (IVIG) without significant improvement of dysphagia. Initially requiring nasogastric (NG) tube feeding, she was later advanced to Percutaneous Endoscopic Gastrostomy (PEG) tube placement due to recurrent aspiration with dysphagia. Endoscopy demonstrated LA Grade A reflux esophagitis, gastritis, and duodenal erosions without bleeding.
Discussion: Rapidly progressive dysphagia is a poor prognostic sign of Dermatomyositis, studies show that the mortality rate is high in patients who required percutaneous endoscopic gastrostomy. A multidisciplinary team approach including nutritionists, speech and language therapists, gastroenterologists, rheumatologists, and neurologist is important for better outcomes.

Figure: Figure A. LA Grade A reflux esophagitis with no bleeding; B. Gastritis; C.PEG tube placement; D. Duodenal erosions without bleeding.
Disclosures:
Khandokar Talib indicated no relevant financial relationships.
Khaleeq Siddiqui indicated no relevant financial relationships.
Yasir Ahmed indicated no relevant financial relationships.
Tasnima Elahi indicated no relevant financial relationships.
Leslie Bank indicated no relevant financial relationships.
Khandokar A. Talib, MD1, Khaleeq Siddiqui, MD2, Yasir Ahmed, MD2, Tasnima Elahi, MD3, Leslie Bank, MD2. P0509 - A Case of Rapidly Progressive Severe Dysphagia in a Patient With Dermatomyositis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
