Sunday Poster Session
Category: Esophagus
P0510 - Bullous Pemphigoid with Esophageal Involvement: A Rare Manifestation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Dirin Ukwade, MD
University of Illinois Chicago
Chicago, IL
Presenting Author(s)
Dirin Ukwade, MD1, Michael Siegel, DO2, Krutika Lakhoo, MD2, Asim Shuja, MD1
1University of Illinois Chicago, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL
Introduction: Bullous pemphigoid (BP) is an autoimmune disease that is known to more commonly affect the skin. Less frequently it can affect mucosal membranes including the gastrointestinal (GI) tract. We present a rare case of BP with esophageal involvement presenting as an upper gastrointestinal bleed (UGIB).
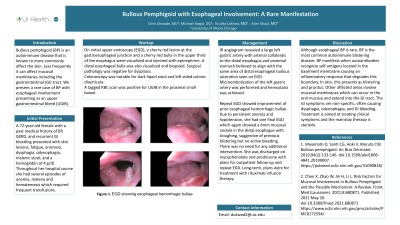
Case Description/Methods: A 72-year-old female with a past medical history of BP, GERD, and recurrent GI bleeding presented with skin lesions, fatigue, anorexia, dysphagia, odynophagia, melenic stool, and a hgb of 4 g/dl. Throughout her hospital course she had several episodes of anemia, melena and hematemesis which required frequent transfusions. Due to concern for active UGIB she underwent multiple studies. On initial upper endoscopy (EGD), a cherry red lesion at the gastroesophageal junction and a cherry red bulla in the upper third of the esophagus were visualized and injected with epinephrine. A distal esophageal bulla was also visualized and biopsied. Surgical pathology was negative for dysplasia. Colonoscopy was notable for dark liquid stool and left sided colonic diverticula. A tagged RBC scan was positive for UGIB in the proximal small bowel. IR angiogram revealed a large left gastric artery with arterial collaterals to the distal esophagus and proximal stomach believed to align with the same area of distal esophageal bullous ulceration seen on EGD. Microembolization of the left gastric artery was performed and hemostasis was achieved. Repeat EGD showed improvement of prior esophageal hemorrhagic bullae. Due to persistent anemia and hypotension, she had one final EGD which again showed a 6mm mucosal nodule in the distal esophagus with sloughing, suggestive of previous blistering but no active bleeding. There was no need for any additional intervention. She was discharged on mycophenolate and prednisone with plans for outpatient follow-up and repeat EGD. Long-term, she was treated with rituximab infusion therapy.
Discussion: Although esophageal BP is rare, BP is the most common autoimmune blistering disease. BP manifests when autoantibodies recognize self-antigens located in the basement membrane causing an inflammatory response that degrades this boundary. In skin, this presents as blistering and pruritus. Other affected areas involve mucosal membranes which can occur in the oral mucosa and extend into the GI tract. The GI symptoms are non-specific, often causing dysphagia, odynophagia, and GI bleeding. Treatment is aimed at treating clinical symptoms and the mainstay therapy is steroids.

Disclosures:
Dirin Ukwade, MD1, Michael Siegel, DO2, Krutika Lakhoo, MD2, Asim Shuja, MD1. P0510 - Bullous Pemphigoid with Esophageal Involvement: A Rare Manifestation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Illinois Chicago, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL
Introduction: Bullous pemphigoid (BP) is an autoimmune disease that is known to more commonly affect the skin. Less frequently it can affect mucosal membranes including the gastrointestinal (GI) tract. We present a rare case of BP with esophageal involvement presenting as an upper gastrointestinal bleed (UGIB).
Case Description/Methods: A 72-year-old female with a past medical history of BP, GERD, and recurrent GI bleeding presented with skin lesions, fatigue, anorexia, dysphagia, odynophagia, melenic stool, and a hgb of 4 g/dl. Throughout her hospital course she had several episodes of anemia, melena and hematemesis which required frequent transfusions. Due to concern for active UGIB she underwent multiple studies. On initial upper endoscopy (EGD), a cherry red lesion at the gastroesophageal junction and a cherry red bulla in the upper third of the esophagus were visualized and injected with epinephrine. A distal esophageal bulla was also visualized and biopsied. Surgical pathology was negative for dysplasia. Colonoscopy was notable for dark liquid stool and left sided colonic diverticula. A tagged RBC scan was positive for UGIB in the proximal small bowel. IR angiogram revealed a large left gastric artery with arterial collaterals to the distal esophagus and proximal stomach believed to align with the same area of distal esophageal bullous ulceration seen on EGD. Microembolization of the left gastric artery was performed and hemostasis was achieved. Repeat EGD showed improvement of prior esophageal hemorrhagic bullae. Due to persistent anemia and hypotension, she had one final EGD which again showed a 6mm mucosal nodule in the distal esophagus with sloughing, suggestive of previous blistering but no active bleeding. There was no need for any additional intervention. She was discharged on mycophenolate and prednisone with plans for outpatient follow-up and repeat EGD. Long-term, she was treated with rituximab infusion therapy.
Discussion: Although esophageal BP is rare, BP is the most common autoimmune blistering disease. BP manifests when autoantibodies recognize self-antigens located in the basement membrane causing an inflammatory response that degrades this boundary. In skin, this presents as blistering and pruritus. Other affected areas involve mucosal membranes which can occur in the oral mucosa and extend into the GI tract. The GI symptoms are non-specific, often causing dysphagia, odynophagia, and GI bleeding. Treatment is aimed at treating clinical symptoms and the mainstay therapy is steroids.

Figure: Esophagus with mucosal sloughing and nodule
Disclosures:
Dirin Ukwade indicated no relevant financial relationships.
Michael Siegel indicated no relevant financial relationships.
Krutika Lakhoo indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
Dirin Ukwade, MD1, Michael Siegel, DO2, Krutika Lakhoo, MD2, Asim Shuja, MD1. P0510 - Bullous Pemphigoid with Esophageal Involvement: A Rare Manifestation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
