Sunday Poster Session
Category: Esophagus
P0514 - When Diabetes Takes Its Toll: Uncontrolled Diabetes Mellitus and Melena
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Saqr Alsakarneh, MD
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Saqr Alsakarneh, MD1, Fouad Jaber, MD1, Anika Mittal, BA2, Yassine Kilani, MD3, Mohammed Jaber, MD4, Ali O.. Ibrahim, MD1, John Campbell, MD1, Muhammad Shah Miran, MD1, Hassan Ghoz, MD1
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Kansas City, MO; 3Lincoln Medical Center, New York, NY; 4Al-Balqa Applied University, School of Medicine, Salt, Al Balqa', Jordan
Introduction: Acute esophageal necrosis (AEN) or black esophagus is a rare cause of gastrointestinal bleeding with significant mortality. Risk factors include male gender, sepsis, uncontrolled diabetes mellitus, cardiovascular disease, renal insufficiency, gastric outlet obstruction, and malnutrition. We report a case of a 54-year-old female with distal AEN that presented with melena.
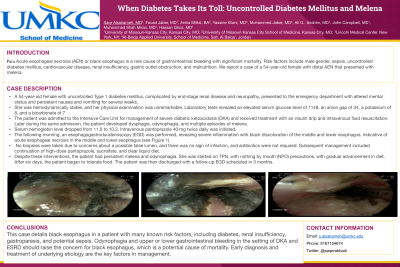
Case Description/Methods: A 54-year-old female with uncontrolled Type 1 diabetes mellitus, complicated by end-stage renal disease and neuropathy, presented to the emergency department with altered mental status and persistent nausea and vomiting for several weeks. She was hemodynamically stable, and her physical examination was unremarkable. Laboratory tests revealed an elevated serum glucose level of 1149, an anion gap of 34, a potassium of 8, and a bicarbonate of 7. The patient was admitted to the Intensive Care Unit for management of severe diabetic ketoacidosis (DKA) and received treatment with an insulin drip and intravenous fluid resuscitation. Later during the same admission, the patient developed dysphagia, odynophagia, and multiple episodes of melena. Serum hemoglobin level dropped from 11.0 to 10.2. Intravenous pantoprazole 40 mg twice daily was initiated. The following morning, an esophagogastroduodenoscopy (EGD) was performed, revealing severe inflammation with black discoloration of the middle and lower esophagus, indicative of acute esophageal necrosis in the middle and lower esophagus (see Figure 1). No biopsies were taken due to concerns about a possible false lumen, and there was no sign of infection, and antibiotics were not required. Subsequent management included continuation of high-dose pantoprazole, sucralfate, and clear liquid diet. Despite these interventions, the patient had persistent melena and odynophagia. She was started on TPN, with nothing by mouth (NPO) precautions, with gradual advancement in diet. After six days, the patient began to tolerate food. The patient was then discharged with a follow-up EGD scheduled in 3 months.
Discussion: This case details black esophagus in a patient with many known risk factors, including diabetes, renal insufficiency, gastroparesis, and potential sepsis. Odynophagia and upper or lower gastrointestinal bleeding in the setting of DKA and ESRD should raise the concern for black esophagus, which is a potential cause of mortality. Early diagnosis and treatment of underlying etiology are the key factors in management.

Disclosures:
Saqr Alsakarneh, MD1, Fouad Jaber, MD1, Anika Mittal, BA2, Yassine Kilani, MD3, Mohammed Jaber, MD4, Ali O.. Ibrahim, MD1, John Campbell, MD1, Muhammad Shah Miran, MD1, Hassan Ghoz, MD1. P0514 - When Diabetes Takes Its Toll: Uncontrolled Diabetes Mellitus and Melena, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Kansas City, MO; 3Lincoln Medical Center, New York, NY; 4Al-Balqa Applied University, School of Medicine, Salt, Al Balqa', Jordan
Introduction: Acute esophageal necrosis (AEN) or black esophagus is a rare cause of gastrointestinal bleeding with significant mortality. Risk factors include male gender, sepsis, uncontrolled diabetes mellitus, cardiovascular disease, renal insufficiency, gastric outlet obstruction, and malnutrition. We report a case of a 54-year-old female with distal AEN that presented with melena.
Case Description/Methods: A 54-year-old female with uncontrolled Type 1 diabetes mellitus, complicated by end-stage renal disease and neuropathy, presented to the emergency department with altered mental status and persistent nausea and vomiting for several weeks. She was hemodynamically stable, and her physical examination was unremarkable. Laboratory tests revealed an elevated serum glucose level of 1149, an anion gap of 34, a potassium of 8, and a bicarbonate of 7. The patient was admitted to the Intensive Care Unit for management of severe diabetic ketoacidosis (DKA) and received treatment with an insulin drip and intravenous fluid resuscitation. Later during the same admission, the patient developed dysphagia, odynophagia, and multiple episodes of melena. Serum hemoglobin level dropped from 11.0 to 10.2. Intravenous pantoprazole 40 mg twice daily was initiated. The following morning, an esophagogastroduodenoscopy (EGD) was performed, revealing severe inflammation with black discoloration of the middle and lower esophagus, indicative of acute esophageal necrosis in the middle and lower esophagus (see Figure 1). No biopsies were taken due to concerns about a possible false lumen, and there was no sign of infection, and antibiotics were not required. Subsequent management included continuation of high-dose pantoprazole, sucralfate, and clear liquid diet. Despite these interventions, the patient had persistent melena and odynophagia. She was started on TPN, with nothing by mouth (NPO) precautions, with gradual advancement in diet. After six days, the patient began to tolerate food. The patient was then discharged with a follow-up EGD scheduled in 3 months.
Discussion: This case details black esophagus in a patient with many known risk factors, including diabetes, renal insufficiency, gastroparesis, and potential sepsis. Odynophagia and upper or lower gastrointestinal bleeding in the setting of DKA and ESRD should raise the concern for black esophagus, which is a potential cause of mortality. Early diagnosis and treatment of underlying etiology are the key factors in management.

Figure: Esophagogastroduodenoscopy revealed Severe inflammation with black discoloration of the middle (A, B) and lower esophagus (C) consistent with acute esophageal necrosis (black esophagus)
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Anika Mittal indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Mohammed Jaber indicated no relevant financial relationships.
Ali Ibrahim indicated no relevant financial relationships.
John Campbell indicated no relevant financial relationships.
Muhammad Shah Miran indicated no relevant financial relationships.
Hassan Ghoz indicated no relevant financial relationships.
Saqr Alsakarneh, MD1, Fouad Jaber, MD1, Anika Mittal, BA2, Yassine Kilani, MD3, Mohammed Jaber, MD4, Ali O.. Ibrahim, MD1, John Campbell, MD1, Muhammad Shah Miran, MD1, Hassan Ghoz, MD1. P0514 - When Diabetes Takes Its Toll: Uncontrolled Diabetes Mellitus and Melena, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
