Sunday Poster Session
Category: Functional Bowel Disease
P0522 - The Gut Microbiome and Symptoms in Irritable Bowel Syndrome
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Kendra Kamp, PhD, RN
University of Washington
Seattle, WA
Presenting Author(s)
Award: Presidential Poster Award
Kendra Kamp, PhD, RN1, Anna M. Plantinga, PhD2, Kevin C. Cain, PhD1, Robert Burr, MS, PhD3, Qinglong Wu, PhD4, Sik Yu So, PhD4, Shyam Badu, PhD4, Tor Savidge, PhD4, Robert Shulman, MD4, Margaret E. Heitkemper, BSN, PhD1
1University of Washington, Seattle, WA; 2Williams College, Williamstown, MA; 3University of Washington, Seattle, Seattle, WA; 4Baylor College of Medicine, Houston, TX
Introduction: Irritable bowel syndrome (IBS), a disorder of gut-brain interaction, is associated with abdominal pain and stool frequency/character; alterations in gut microbiome composition also have been described. We sought to test whether taxa identified as differentially abundant between women with IBS vs healthy control (HC) women are associated with daily symptom (abdominal pain, constipation and diarrhea) severity within the IBS group.
Methods: Women (age 18-45 yr) were recruited from the community and gastroenterology clinics in the Pacific Northwest. They completed a 28-day symptom diary in which symptom intensity was rated. Participants collected a stool sample between days 3-8 of their menstrual cycle and completed a 3 day food record during this time. Participants also completed questionnaires regarding demographic and clinical characteristics. 16S rRNA gene sequencing for bacterial identification was conducted on the stool samples by the Texas Children’s Hospital Microbiome Center. Symptoms from the three days following stool collection were used for the purposes of analyses. Linear regression analysis was used to compare IBS and HC groups.
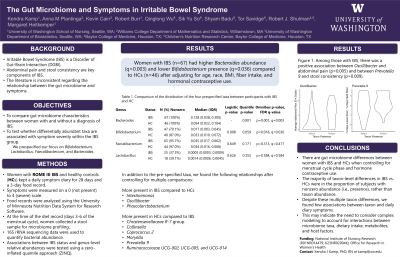
Results: Women with IBS (n=67) had greater Bacteroides abundance (p=0.003, q=0.007) and lower Bifidobacterium abundance (p< 0.001, q=0.004) compared to HCs (n=46) after adjusting for age, race, body mass index, fiber intake, and hormonal contraceptive use. In addition to the prespecified taxa, [Eubacterium] fissicatena group, Eisenbergiella, Flavonifractor, Intestimonas, Oscillibacter, and Phascolarcobacterium had increased abundance in IBS vs HCs. In addition, Christensenellaceae R-7 group, Collinsella, Coprococcus 2, Moryella, Prevotella 9, Ruminococcaceae UCG-002, and Ruminococcaceae UCG-005 had decreased abundance in IBS vs HCs. Among those with IBS, there was an association between Oscillibacter abundance and abdominal pain (p=0.001, q=0.032) and between Prevotella 9 abundance and loose stool consistency (p=0.001, q=0.032).
Discussion: There are gut microbiome differences between women with IBS and HCs when controlling for menstrual cycle phase, fiber intake, and hormone contraceptive use. Despite these multiple taxon differences, we found few associations between individual taxon and concurrent daily diary IBS symptoms. This may indicate the need to consider complex modeling to account for interactions between microbiome taxa, dietary intake, metabolites, and host factors.
Disclosures:
Kendra Kamp, PhD, RN1, Anna M. Plantinga, PhD2, Kevin C. Cain, PhD1, Robert Burr, MS, PhD3, Qinglong Wu, PhD4, Sik Yu So, PhD4, Shyam Badu, PhD4, Tor Savidge, PhD4, Robert Shulman, MD4, Margaret E. Heitkemper, BSN, PhD1. P0522 - The Gut Microbiome and Symptoms in Irritable Bowel Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Kendra Kamp, PhD, RN1, Anna M. Plantinga, PhD2, Kevin C. Cain, PhD1, Robert Burr, MS, PhD3, Qinglong Wu, PhD4, Sik Yu So, PhD4, Shyam Badu, PhD4, Tor Savidge, PhD4, Robert Shulman, MD4, Margaret E. Heitkemper, BSN, PhD1
1University of Washington, Seattle, WA; 2Williams College, Williamstown, MA; 3University of Washington, Seattle, Seattle, WA; 4Baylor College of Medicine, Houston, TX
Introduction: Irritable bowel syndrome (IBS), a disorder of gut-brain interaction, is associated with abdominal pain and stool frequency/character; alterations in gut microbiome composition also have been described. We sought to test whether taxa identified as differentially abundant between women with IBS vs healthy control (HC) women are associated with daily symptom (abdominal pain, constipation and diarrhea) severity within the IBS group.
Methods: Women (age 18-45 yr) were recruited from the community and gastroenterology clinics in the Pacific Northwest. They completed a 28-day symptom diary in which symptom intensity was rated. Participants collected a stool sample between days 3-8 of their menstrual cycle and completed a 3 day food record during this time. Participants also completed questionnaires regarding demographic and clinical characteristics. 16S rRNA gene sequencing for bacterial identification was conducted on the stool samples by the Texas Children’s Hospital Microbiome Center. Symptoms from the three days following stool collection were used for the purposes of analyses. Linear regression analysis was used to compare IBS and HC groups.
Results: Women with IBS (n=67) had greater Bacteroides abundance (p=0.003, q=0.007) and lower Bifidobacterium abundance (p< 0.001, q=0.004) compared to HCs (n=46) after adjusting for age, race, body mass index, fiber intake, and hormonal contraceptive use. In addition to the prespecified taxa, [Eubacterium] fissicatena group, Eisenbergiella, Flavonifractor, Intestimonas, Oscillibacter, and Phascolarcobacterium had increased abundance in IBS vs HCs. In addition, Christensenellaceae R-7 group, Collinsella, Coprococcus 2, Moryella, Prevotella 9, Ruminococcaceae UCG-002, and Ruminococcaceae UCG-005 had decreased abundance in IBS vs HCs. Among those with IBS, there was an association between Oscillibacter abundance and abdominal pain (p=0.001, q=0.032) and between Prevotella 9 abundance and loose stool consistency (p=0.001, q=0.032).
Discussion: There are gut microbiome differences between women with IBS and HCs when controlling for menstrual cycle phase, fiber intake, and hormone contraceptive use. Despite these multiple taxon differences, we found few associations between individual taxon and concurrent daily diary IBS symptoms. This may indicate the need to consider complex modeling to account for interactions between microbiome taxa, dietary intake, metabolites, and host factors.
Disclosures:
Kendra Kamp indicated no relevant financial relationships.
Anna Plantinga indicated no relevant financial relationships.
Kevin Cain indicated no relevant financial relationships.
Robert Burr indicated no relevant financial relationships.
Qinglong Wu: patent applications – Intellectual Property/Patents.
Sik Yu So indicated no relevant financial relationships.
Shyam Badu indicated no relevant financial relationships.
Tor Savidge: BioFire – Advisory Committee/Board Member, Grant/Research Support. patent applications – Intellectual Property/Patents. Rebiotix – Advisory Committee/Board Member, Grant/Research Support.
Robert Shulman: Cairn Diagnostics – Grant/Research Support. Rome Foundation – Intellectual Property/Patents.
Margaret Heitkemper indicated no relevant financial relationships.
Kendra Kamp, PhD, RN1, Anna M. Plantinga, PhD2, Kevin C. Cain, PhD1, Robert Burr, MS, PhD3, Qinglong Wu, PhD4, Sik Yu So, PhD4, Shyam Badu, PhD4, Tor Savidge, PhD4, Robert Shulman, MD4, Margaret E. Heitkemper, BSN, PhD1. P0522 - The Gut Microbiome and Symptoms in Irritable Bowel Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

