Sunday Poster Session
Category: Functional Bowel Disease
P0533 - A Virtual Integrated Care Program Improves Patient Outcomes, Engagement, and Satisfaction at Reduced Costs: A Prospective Trial
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Sameer K. Berry, MD, MBA
New York Gastroenterology Associates
new york , NY
Presenting Author(s)
Award: Presidential Poster Award
Sameer K. Berry, MD, MBA1, Jeffrey Berinstein, MD, MSc2, David J. Cook, MD3, Michael Lahm, BA4, Walter W. Chan, MD, MPH5, John I. Allen, MD, MBA6, William D. Chey, MD6
1New York Gastroenterology Associates, New York, NY; 2University of Michigan Hospital, Ann Arbor, MI; 3Mayo Foundation for Medical Education and Research, Rochester, MN; 4Optum, Eden Prairie, MN; 5Brigham and Women's Hospital, Boston, MA; 6University of Michigan, Ann Arbor, MI
Introduction: Disorders of gut-brain interaction (DGBI) are characterized by chronic gastrointestinal (GI) symptoms without structural abnormalities. DGBIs affect > 20% of the United States population, costing over $30 billion annually. Despite the high prevalence, only 10–25% of patients with GI symptoms seek care, in part related to poor access to timely, high-quality care. This highlights the need for innovative multidisciplinary care models in partnership with traditional clinic-based GI care to address the unmet needs of these complex patients.
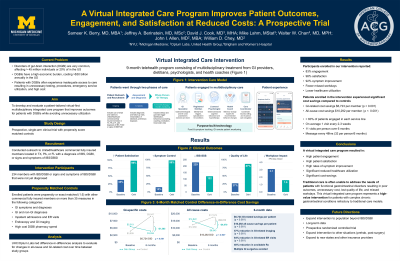
Methods: We performed a prospective, single-arm clinical trial with 1:5 propensity-score matched controls to evaluate the effectiveness of a virtual integrated-care program on clinical outcomes, patient satisfaction, and costs in patients with DGBIs as well as patients with GI symptoms without a formal DGBI diagnosis. Analyses was performed using a GI visit as the index date for the control group and enrollment in the virtual integrated-care program for the intervention group. Cost and utilization analyses were performed by Optum Labs (United Healthcare Group) using their claims database. Difference-in-differences analysis was used to evaluate changes in all-cause and GI-related cost over time between study groups.
Results: Among 234 participants enrolled in the virtual integrated-care program, 83% remained engaged, 98% reported satisfaction, 92% reported symptom improvement, along with 1.3 fewer missed workdays reported over 6 months. After 6 months, patients enrolled in the virtual integrated-care program had significantly lower GI-related costs ($3,934 vs. $9,047, p< 0.0001) and all-cause costs ($9,843 vs $17,573, p=0.0033) compared to propensity-matched controls (Figure 1). Difference-in-difference analyses demonstrated GI-related cost-savings of $6,723 (p< 0.0001) and all-cause savings of $10,292 (p=0.00076). These savings were driven predominantly by significant reduction in avoidable GI-related ED visits (8% vs 21%, p< 0.0001), GI-related imaging (20% vs 47%, p< 0.001), endoscopy (15% vs 68%, p < 0.0001), and all-cause ED visits (20% vs 28%, p=0.0087). These cost savings and reduction in avoidable utilization were sustained at 9 months.
Discussion: A virtual integrated-care program in partnership with traditional GI practices resulted in high patient engagement, satisfaction, symptom improvement, reduced healthcare utilization, and statistically significant cost-savings for patients with DGBIs compared to propensity-matched controls.
Disclosures:
Sameer K. Berry, MD, MBA1, Jeffrey Berinstein, MD, MSc2, David J. Cook, MD3, Michael Lahm, BA4, Walter W. Chan, MD, MPH5, John I. Allen, MD, MBA6, William D. Chey, MD6. P0533 - A Virtual Integrated Care Program Improves Patient Outcomes, Engagement, and Satisfaction at Reduced Costs: A Prospective Trial, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Sameer K. Berry, MD, MBA1, Jeffrey Berinstein, MD, MSc2, David J. Cook, MD3, Michael Lahm, BA4, Walter W. Chan, MD, MPH5, John I. Allen, MD, MBA6, William D. Chey, MD6
1New York Gastroenterology Associates, New York, NY; 2University of Michigan Hospital, Ann Arbor, MI; 3Mayo Foundation for Medical Education and Research, Rochester, MN; 4Optum, Eden Prairie, MN; 5Brigham and Women's Hospital, Boston, MA; 6University of Michigan, Ann Arbor, MI
Introduction: Disorders of gut-brain interaction (DGBI) are characterized by chronic gastrointestinal (GI) symptoms without structural abnormalities. DGBIs affect > 20% of the United States population, costing over $30 billion annually. Despite the high prevalence, only 10–25% of patients with GI symptoms seek care, in part related to poor access to timely, high-quality care. This highlights the need for innovative multidisciplinary care models in partnership with traditional clinic-based GI care to address the unmet needs of these complex patients.
Methods: We performed a prospective, single-arm clinical trial with 1:5 propensity-score matched controls to evaluate the effectiveness of a virtual integrated-care program on clinical outcomes, patient satisfaction, and costs in patients with DGBIs as well as patients with GI symptoms without a formal DGBI diagnosis. Analyses was performed using a GI visit as the index date for the control group and enrollment in the virtual integrated-care program for the intervention group. Cost and utilization analyses were performed by Optum Labs (United Healthcare Group) using their claims database. Difference-in-differences analysis was used to evaluate changes in all-cause and GI-related cost over time between study groups.
Results: Among 234 participants enrolled in the virtual integrated-care program, 83% remained engaged, 98% reported satisfaction, 92% reported symptom improvement, along with 1.3 fewer missed workdays reported over 6 months. After 6 months, patients enrolled in the virtual integrated-care program had significantly lower GI-related costs ($3,934 vs. $9,047, p< 0.0001) and all-cause costs ($9,843 vs $17,573, p=0.0033) compared to propensity-matched controls (Figure 1). Difference-in-difference analyses demonstrated GI-related cost-savings of $6,723 (p< 0.0001) and all-cause savings of $10,292 (p=0.00076). These savings were driven predominantly by significant reduction in avoidable GI-related ED visits (8% vs 21%, p< 0.0001), GI-related imaging (20% vs 47%, p< 0.001), endoscopy (15% vs 68%, p < 0.0001), and all-cause ED visits (20% vs 28%, p=0.0087). These cost savings and reduction in avoidable utilization were sustained at 9 months.
Discussion: A virtual integrated-care program in partnership with traditional GI practices resulted in high patient engagement, satisfaction, symptom improvement, reduced healthcare utilization, and statistically significant cost-savings for patients with DGBIs compared to propensity-matched controls.
Disclosures:
Sameer Berry indicated no relevant financial relationships.
Jeffrey Berinstein: Bristol Myers Squibb – Consultant. Buhlman Diagnostics – Consultant. Oshi Health – Consultant.
David J. Cook: Optum – Employee.
Michael Lahm: Optum – Employee.
Walter Chan: Phathom Pharmaceutical – Advisory Committee/Board Member. Regeneron Pharmaceutical – Advisory Committee/Board Member. Sanofi Pharmaceutical – Advisory Committee/Board Member.
John I. Allen indicated no relevant financial relationships.
William D. Chey: Commonwealth Diagnostics International – Grant/Research Support. Salix Pharmaceuticals – Advisor or Review Panel Member, Grant/Research Support.
Sameer K. Berry, MD, MBA1, Jeffrey Berinstein, MD, MSc2, David J. Cook, MD3, Michael Lahm, BA4, Walter W. Chan, MD, MPH5, John I. Allen, MD, MBA6, William D. Chey, MD6. P0533 - A Virtual Integrated Care Program Improves Patient Outcomes, Engagement, and Satisfaction at Reduced Costs: A Prospective Trial, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

