Sunday Poster Session
Category: General Endoscopy
P0581 - Inlet Patches: To Biopsy or Not to Biopsy?
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Denisse Camille Dayto, MD
HCA Florida Citrus Hospital
Inverness, FL
Presenting Author(s)
Denisse Camille Dayto, MD1, Andrew Sephien, MD2, Varun Patel, MD1
1HCA Florida Citrus Hospital, Inverness, FL; 2HCA Healthcare/USF Morsani GME Consortium: HCA Florida Citrus Hospital, Inverness, FL
Introduction: Inlet patches (IPs) or heterotopic gastric mucosa are reported with an incidence of 0.3% to 10%. IPs are commonly overlooked on endoscopy and rarely biopsied as most are benign and asymptomatic. Occasionally, few can cause dysphagia, ulceration, stricture formation, and perforation. While rare, literature has reported a predisposition to both Barrett’s esophagus (BE) and adenocarcinoma with 42 cases reported. BE has been shown to have up to four-fold increased risk of IP, with one reported case of synchronous esophageal adenocarcinoma from IP and BE-related dysplasia.
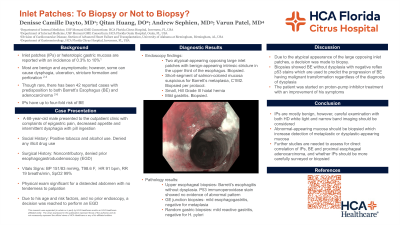
Case Description/Methods: A 68-year-old male with past medical history of alcohol and tobacco dependence presented with complaints of epigastric pain, decreased appetite, and intermittent dysphagia with pill ingestion. Physical exam was notable for non-tender, distended abdomen. He had no prior history of endoscopy. However, due to his age and risk factors, an esophagogastroduodenoscopy (EGD) was performed and revealed a Hill grade III hiatal hernia, multiple patches of gastric ectopic mucosa in the upper third of the esophagus, and two large ectopic gastric mucosal tissue seen at 21 cm from the incisors with atypical darker pigmentation on the periphery. An area with salmon-colored mucosa was also observed with a Prague score of C1M2, raising suspicion for Barrett’s intestinal metaplasia. Four quadrant cold forceps biopsies and random gastric biopsies were performed. Pathology reports of random gastric biopsies showed mild reactive gastritis, negative for H pylori. EG junction biopsy showed mild esophagogastritis, negative for metaplasia. Esophageal biopsy at 21 cm showed Barrett’s esophagitis, negative for dysplasia. However, due to atypical features seen on endoscopy, a p53 immunoperoxidase stain was performed and showed no evidence of abnormal pattern indicative of neoplastic progression. The patient was started on proton-pump inhibitor treatment with an improvement of his symptoms.
Discussion: While IPs are considered benign, biopsies should be considered if any irregular features or atypical locations are noted on EGD to rule out dysplasia. Due to the aberrant appearance of the inlet patch noted, a biopsy was obtained and a p53 immunoperoxidase stain was done to predict the progression of BE having malignant transformation regardless of the diagnosis of dysplasia. Future studies should assess if there is a direct correlation between IP, BE and adenocarcinoma, and whether IPs should be more carefully surveyed or biopsied.

Disclosures:
Denisse Camille Dayto, MD1, Andrew Sephien, MD2, Varun Patel, MD1. P0581 - Inlet Patches: To Biopsy or Not to Biopsy?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA Florida Citrus Hospital, Inverness, FL; 2HCA Healthcare/USF Morsani GME Consortium: HCA Florida Citrus Hospital, Inverness, FL
Introduction: Inlet patches (IPs) or heterotopic gastric mucosa are reported with an incidence of 0.3% to 10%. IPs are commonly overlooked on endoscopy and rarely biopsied as most are benign and asymptomatic. Occasionally, few can cause dysphagia, ulceration, stricture formation, and perforation. While rare, literature has reported a predisposition to both Barrett’s esophagus (BE) and adenocarcinoma with 42 cases reported. BE has been shown to have up to four-fold increased risk of IP, with one reported case of synchronous esophageal adenocarcinoma from IP and BE-related dysplasia.
Case Description/Methods: A 68-year-old male with past medical history of alcohol and tobacco dependence presented with complaints of epigastric pain, decreased appetite, and intermittent dysphagia with pill ingestion. Physical exam was notable for non-tender, distended abdomen. He had no prior history of endoscopy. However, due to his age and risk factors, an esophagogastroduodenoscopy (EGD) was performed and revealed a Hill grade III hiatal hernia, multiple patches of gastric ectopic mucosa in the upper third of the esophagus, and two large ectopic gastric mucosal tissue seen at 21 cm from the incisors with atypical darker pigmentation on the periphery. An area with salmon-colored mucosa was also observed with a Prague score of C1M2, raising suspicion for Barrett’s intestinal metaplasia. Four quadrant cold forceps biopsies and random gastric biopsies were performed. Pathology reports of random gastric biopsies showed mild reactive gastritis, negative for H pylori. EG junction biopsy showed mild esophagogastritis, negative for metaplasia. Esophageal biopsy at 21 cm showed Barrett’s esophagitis, negative for dysplasia. However, due to atypical features seen on endoscopy, a p53 immunoperoxidase stain was performed and showed no evidence of abnormal pattern indicative of neoplastic progression. The patient was started on proton-pump inhibitor treatment with an improvement of his symptoms.
Discussion: While IPs are considered benign, biopsies should be considered if any irregular features or atypical locations are noted on EGD to rule out dysplasia. Due to the aberrant appearance of the inlet patch noted, a biopsy was obtained and a p53 immunoperoxidase stain was done to predict the progression of BE having malignant transformation regardless of the diagnosis of dysplasia. Future studies should assess if there is a direct correlation between IP, BE and adenocarcinoma, and whether IPs should be more carefully surveyed or biopsied.

Figure: Cervical Inlet Patch on Endoscopy
Disclosures:
Denisse Camille Dayto indicated no relevant financial relationships.
Andrew Sephien indicated no relevant financial relationships.
Varun Patel indicated no relevant financial relationships.
Denisse Camille Dayto, MD1, Andrew Sephien, MD2, Varun Patel, MD1. P0581 - Inlet Patches: To Biopsy or Not to Biopsy?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
