Sunday Poster Session
Category: General Endoscopy
P0582 - Third Time Is the Charm: Amyloidosis Diagnosed Through Duodenal Biopsy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Geethanjali Rajagopal, MD
University of Chicago Medical Center
Chicago, IL
Presenting Author(s)
Geethanjali Rajagopal, MD1, Grace E.. Kim, MD2, Vijaya Rao, MD2
1University of Chicago Medical Center, Chicago, IL; 2University of Chicago, Chicago, IL
Introduction: Amyloidosis results from extracellular deposition of misfolded proteins and can be systemic or localized, and the gastrointestinal (GI) system can be involved in both types. However, direct visualization of amyloid deposition on pathology from the GI tract is uncommon. [1] We present a unique case of a newly identified amyloidosis diagnosed via duodenal biopsies in a patient with prior endoscopic evaluations.
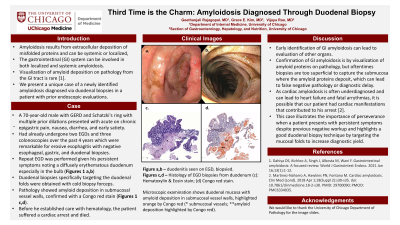
Case Description/Methods: A 70-year-old male with GERD and Schatzki's ring with multiple prior dilations presented with acute on chronic epigastric pain, nausea, diarrhea, and early satiety. He had already undergone two EGDs and three colonoscopies for his symptoms over the past 4 years which showed erosive esophagitis and a small colorectal tubular adenoma respectively. No other remarkable findings were noted with previous esophageal, gastric, and duodenal biopsies. A repeat EGD was performed given his persistent symptoms noting a diffusely erythematous duodenum especially in the bulb (Figures 1 a,b), thus a set of duodenal biopsies specifically targeting the duodenal folds was obtained with cold biopsy forceps. Pathology showed amyloid deposition in submucosal vessel walls, confirmed with a Congo red stain (Figures 1 c,d). Before he established care with hematology, the patient suffered a cardiac arrest and died.
Discussion: Early identification of GI amyloidosis can lead to evaluation of other organs. Cardiac amyloidosis is often underdiagnosed and can lead to complications like heart failure and fatal arrythmias. [2] It is possible that our patient had cardiac manifestations that contributed to his arrest, but the exact cause of his arrest is unknown.
Visualization of amyloid proteins on pathology confirms the diagnosis of GI amyloidosis, but oftentimes biopsies are too superficial to capture the submucosa where the amyloid proteins deposit, leading to false negative pathology and subsequent diagnostic delay. Targeting the mucosal folds during duodenal biopsies will increase diagnostic yield and can lead to a definitive diagnosis.
1. Dahiya DS, Kichloo A, Singh J, Albosta M, Wani F. Gastrointestinal amyloidosis: A focused review. World J Gastrointest Endosc. 2021 Jan 16;13(1):1-12.
2. Martinez-Naharro A, Hawkins PN, Fontana M. Cardiac amyloidosis. Clin Med (Lond). 2018 Apr 1;18(Suppl 2):s30-s35.

Disclosures:
Geethanjali Rajagopal, MD1, Grace E.. Kim, MD2, Vijaya Rao, MD2. P0582 - Third Time Is the Charm: Amyloidosis Diagnosed Through Duodenal Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Chicago Medical Center, Chicago, IL; 2University of Chicago, Chicago, IL
Introduction: Amyloidosis results from extracellular deposition of misfolded proteins and can be systemic or localized, and the gastrointestinal (GI) system can be involved in both types. However, direct visualization of amyloid deposition on pathology from the GI tract is uncommon. [1] We present a unique case of a newly identified amyloidosis diagnosed via duodenal biopsies in a patient with prior endoscopic evaluations.
Case Description/Methods: A 70-year-old male with GERD and Schatzki's ring with multiple prior dilations presented with acute on chronic epigastric pain, nausea, diarrhea, and early satiety. He had already undergone two EGDs and three colonoscopies for his symptoms over the past 4 years which showed erosive esophagitis and a small colorectal tubular adenoma respectively. No other remarkable findings were noted with previous esophageal, gastric, and duodenal biopsies. A repeat EGD was performed given his persistent symptoms noting a diffusely erythematous duodenum especially in the bulb (Figures 1 a,b), thus a set of duodenal biopsies specifically targeting the duodenal folds was obtained with cold biopsy forceps. Pathology showed amyloid deposition in submucosal vessel walls, confirmed with a Congo red stain (Figures 1 c,d). Before he established care with hematology, the patient suffered a cardiac arrest and died.
Discussion: Early identification of GI amyloidosis can lead to evaluation of other organs. Cardiac amyloidosis is often underdiagnosed and can lead to complications like heart failure and fatal arrythmias. [2] It is possible that our patient had cardiac manifestations that contributed to his arrest, but the exact cause of his arrest is unknown.
Visualization of amyloid proteins on pathology confirms the diagnosis of GI amyloidosis, but oftentimes biopsies are too superficial to capture the submucosa where the amyloid proteins deposit, leading to false negative pathology and subsequent diagnostic delay. Targeting the mucosal folds during duodenal biopsies will increase diagnostic yield and can lead to a definitive diagnosis.
1. Dahiya DS, Kichloo A, Singh J, Albosta M, Wani F. Gastrointestinal amyloidosis: A focused review. World J Gastrointest Endosc. 2021 Jan 16;13(1):1-12.
2. Martinez-Naharro A, Hawkins PN, Fontana M. Cardiac amyloidosis. Clin Med (Lond). 2018 Apr 1;18(Suppl 2):s30-s35.

Figure: Figure 1a,b – Duodenitis seen on EGD, biopsied. Figures c,d: Histology of EGD biopsies from duodenum (c): Hematoxylin & Eosin stain; (d) Congo red stain. Microscopic examination shows duodenal mucosa with amyloid deposition in submucosal vessel walls, highlighted orange by Congo red (* submucosal vessels; ** amyloid deposition highlighted by Congo red).
Disclosures:
Geethanjali Rajagopal indicated no relevant financial relationships.
Grace Kim indicated no relevant financial relationships.
Vijaya Rao indicated no relevant financial relationships.
Geethanjali Rajagopal, MD1, Grace E.. Kim, MD2, Vijaya Rao, MD2. P0582 - Third Time Is the Charm: Amyloidosis Diagnosed Through Duodenal Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
