Sunday Poster Session
Category: General Endoscopy
P0587 - An Incidental Diagnosis of an Invisible Gastric Adenocarcinoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jaya Bommireddipally, MD
Tulane University
New Orleans, LA
Presenting Author(s)
Jaya Bommireddipally, MD1, Jowana Saba, MD2, Vance Hartke, MD3, Benjamin A. Guider, MD2
1Tulane University, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA; 3Tulane Medical Center, New Orleans, LA
Introduction: Gastric adenocarcinoma (GA) is a leading cause of cancer-related mortality in the world. GA diagnosis is made with an esophagogastroduodenoscopy (EGD) showing a mass or ulcer. In more subtle cases, an enlarged fold, nodule, or erosion is visible. We present a unique incidental finding of an invisible gastric adenocarcinoma during a screening EGD in a patient with cirrhosis.
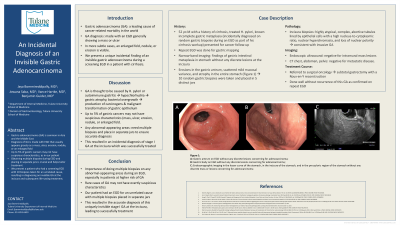
Case Description/Methods: A 52-year-old male with a history of cirrhosis, treated Helicobacter pylori, and known incomplete gastric metaplasia presented to the clinic for cancer follow-up. The patient’s incomplete metaplasia was diagnosed incidentally on random gastric biopsies during an EGD as part of his cirrhosis workup. He then had a repeat EGD for gastric mapping. Narrow-band imaging revealed classic findings of gastric intestinal metaplasia throughout the stomach without any discrete lesions identified at the incisura. Due to erosions in the gastric antrum, scattered mild mucosal variance, and atrophy seen in the entire stomach (Figure 1), 10 random gastric biopsies were taken. On pathology review, the biopsies of the incisura showed highly atypical, complex, abortive tubules lined by epithelial cells with a high nucleus-to-cytoplasmic ratio, nuclear hyperchromasia, and loss of nuclear polarity, consistent with invasive GA. Of note, all biopsies from the gastric mapping were placed in 5 distinct jars, as opposed to the usual 2 jars, which helped identify the isolated GA at the incisura. An endoscopic ultrasound was negative for intramural mass lesions. Computerized tomography (CT) of the chest, abdomen, and pelvis was negative for metastatic disease. He was referred to surgical oncology and had a subtotal gastrectomy with a Roux-en-Y reconstruction. He has since done well without recurrence of this GA as confirmed on repeat EGD.
Discussion: This case shows the importance of doing multiple biopsies on any abnormal-appearing areas during an EGD, especially in patients at higher risk of GA. Rare cases of GA may not have overtly suspicious characteristics, such as in this case. Our patient had an EGD for an unrelated cause with multiple biopsies placed in separate jars. This resulted in the accurate diagnosis of this uniquely invisible stage I GA at the incisura which was successfully treated.

Disclosures:
Jaya Bommireddipally, MD1, Jowana Saba, MD2, Vance Hartke, MD3, Benjamin A. Guider, MD2. P0587 - An Incidental Diagnosis of an Invisible Gastric Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tulane University, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA; 3Tulane Medical Center, New Orleans, LA
Introduction: Gastric adenocarcinoma (GA) is a leading cause of cancer-related mortality in the world. GA diagnosis is made with an esophagogastroduodenoscopy (EGD) showing a mass or ulcer. In more subtle cases, an enlarged fold, nodule, or erosion is visible. We present a unique incidental finding of an invisible gastric adenocarcinoma during a screening EGD in a patient with cirrhosis.
Case Description/Methods: A 52-year-old male with a history of cirrhosis, treated Helicobacter pylori, and known incomplete gastric metaplasia presented to the clinic for cancer follow-up. The patient’s incomplete metaplasia was diagnosed incidentally on random gastric biopsies during an EGD as part of his cirrhosis workup. He then had a repeat EGD for gastric mapping. Narrow-band imaging revealed classic findings of gastric intestinal metaplasia throughout the stomach without any discrete lesions identified at the incisura. Due to erosions in the gastric antrum, scattered mild mucosal variance, and atrophy seen in the entire stomach (Figure 1), 10 random gastric biopsies were taken. On pathology review, the biopsies of the incisura showed highly atypical, complex, abortive tubules lined by epithelial cells with a high nucleus-to-cytoplasmic ratio, nuclear hyperchromasia, and loss of nuclear polarity, consistent with invasive GA. Of note, all biopsies from the gastric mapping were placed in 5 distinct jars, as opposed to the usual 2 jars, which helped identify the isolated GA at the incisura. An endoscopic ultrasound was negative for intramural mass lesions. Computerized tomography (CT) of the chest, abdomen, and pelvis was negative for metastatic disease. He was referred to surgical oncology and had a subtotal gastrectomy with a Roux-en-Y reconstruction. He has since done well without recurrence of this GA as confirmed on repeat EGD.
Discussion: This case shows the importance of doing multiple biopsies on any abnormal-appearing areas during an EGD, especially in patients at higher risk of GA. Rare cases of GA may not have overtly suspicious characteristics, such as in this case. Our patient had an EGD for an unrelated cause with multiple biopsies placed in separate jars. This resulted in the accurate diagnosis of this uniquely invisible stage I GA at the incisura which was successfully treated.

Figure: Figure 1: A: Gastric antrum on EGD without any discrete lesions concerning for adenocarcinoma;
B: Gastric body on EGD without any discrete lesions concerning for adenocarcinoma;
C: Endosonographic imaging in the lesser curve of the stomach, in the incisura of the stomach, and in the pre-pyloric region of the stomach without any discrete mass or lesions concerning for adenocarcinoma
B: Gastric body on EGD without any discrete lesions concerning for adenocarcinoma;
C: Endosonographic imaging in the lesser curve of the stomach, in the incisura of the stomach, and in the pre-pyloric region of the stomach without any discrete mass or lesions concerning for adenocarcinoma
Disclosures:
Jaya Bommireddipally indicated no relevant financial relationships.
Jowana Saba indicated no relevant financial relationships.
Vance Hartke indicated no relevant financial relationships.
Benjamin Guider indicated no relevant financial relationships.
Jaya Bommireddipally, MD1, Jowana Saba, MD2, Vance Hartke, MD3, Benjamin A. Guider, MD2. P0587 - An Incidental Diagnosis of an Invisible Gastric Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
