Sunday Poster Session
Category: GI Bleeding
P0599 - COVID-19 in Non-Variceal Upper GI Bleeding: A National Cohort Study
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aizaz Khan, MD
University of Massachusetts Chan Medical School-Baystate
Springfield, Massachusetts
Presenting Author(s)
Aizaz Khan, MD1, Kamesh Gupta, MD2, Victoria Caruso, DO2
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2University of Massachusetts-Chan Baystate Medical Center, Springfield, MA
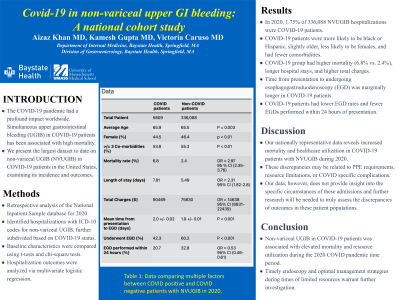
Introduction: Coronavirus disease 2019 (COVID-19) was one of the most devastating pandemic in the modern world. Simultaneous upper gastrointestinal bleeding (UGIB) in patients with COVID-19 infection has been reported to have mortality as high as 41.9%. We present the largest dataset to date on non variceal upper gastrointestinal bleeding (NVUGIB) in patients with COVID-19 in the United States, evaluating incidence and outcomes.
Methods: We conducted a retrospective analysis reviewing the National Inpatient Sample database for hospitalizations that included ICD-10 codes for Upper GI non-variceal bleeding during 2020. These were further subdivided based upon if they had COVID-19. Baseline characteristics were compared using t-test and chi-square tests. Hospitalization outcomes were analyzed using a multivariate logistic regression model to control for age, race, Charlson comorbidity index, intensive care unit (ICU) admission, shock and acute renal failure.
Results: Of 336,088 hospitalizations with NVUGIB in 2020, 5809 (1.75%) patients had concurrent COVID-19. These COVID-19 patients were more likely to be black (19.3% vs 15%, p< 0.01) or hispanic (17.9% vs 9.6%, p< 0.01), were of slightly older age (65.9 vs 65.5, p=0.003), less likely to be females (44.5% vs 46.4%, p< 0.01), and were less likely to have ≥ 3 comorbidities (53.8% vs 55.3%, p< 0.01). COVID-19 group had a higher mortality rate (6.8% vs 2.4%, odds ratio (OR) 2.97, 95% confidence interval (CI): 2.35-3.76), length of stay (5.49 vs 7.81 days, OR 2.31, 1.82-2.8), and total charges for the hospitalization ($90469 vs $75830, OR 14638, OR 6836-22439). Mean time from presentation to undergoing esophagogastroduodenoscopy (EGD) was marginally higher for COVID-19 infected individuals (2.0±.02 days vs 1.9±0.01 days, p< 0.001). NVUGIB patients with COVID-19 patients were less likely to undergo EGD during the hospitalization (42.3% vs 60.2%, p< 0.001) and less likely to have EGD performed within 24 hours of presentation (20.7% vs 32.8%, OR 0.53, 0.46-0.61).
Discussion: Our nationally representative data suggests concurrent NVUGIB in patients with COVID-19 infection significantly increased mortality rates and healthcare utilization. The mortality rate in our study is lesser than the previously reported single center studies. Endoscopy was performed less frequently in COVID-19 patients with NVUGIB, along with a significant delay in time-to-EGD, although we could not provide evidence whether endoscopy was beneficial for these patients.
Disclosures:
Aizaz Khan, MD1, Kamesh Gupta, MD2, Victoria Caruso, DO2. P0599 - COVID-19 in Non-Variceal Upper GI Bleeding: A National Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2University of Massachusetts-Chan Baystate Medical Center, Springfield, MA
Introduction: Coronavirus disease 2019 (COVID-19) was one of the most devastating pandemic in the modern world. Simultaneous upper gastrointestinal bleeding (UGIB) in patients with COVID-19 infection has been reported to have mortality as high as 41.9%. We present the largest dataset to date on non variceal upper gastrointestinal bleeding (NVUGIB) in patients with COVID-19 in the United States, evaluating incidence and outcomes.
Methods: We conducted a retrospective analysis reviewing the National Inpatient Sample database for hospitalizations that included ICD-10 codes for Upper GI non-variceal bleeding during 2020. These were further subdivided based upon if they had COVID-19. Baseline characteristics were compared using t-test and chi-square tests. Hospitalization outcomes were analyzed using a multivariate logistic regression model to control for age, race, Charlson comorbidity index, intensive care unit (ICU) admission, shock and acute renal failure.
Results: Of 336,088 hospitalizations with NVUGIB in 2020, 5809 (1.75%) patients had concurrent COVID-19. These COVID-19 patients were more likely to be black (19.3% vs 15%, p< 0.01) or hispanic (17.9% vs 9.6%, p< 0.01), were of slightly older age (65.9 vs 65.5, p=0.003), less likely to be females (44.5% vs 46.4%, p< 0.01), and were less likely to have ≥ 3 comorbidities (53.8% vs 55.3%, p< 0.01). COVID-19 group had a higher mortality rate (6.8% vs 2.4%, odds ratio (OR) 2.97, 95% confidence interval (CI): 2.35-3.76), length of stay (5.49 vs 7.81 days, OR 2.31, 1.82-2.8), and total charges for the hospitalization ($90469 vs $75830, OR 14638, OR 6836-22439). Mean time from presentation to undergoing esophagogastroduodenoscopy (EGD) was marginally higher for COVID-19 infected individuals (2.0±.02 days vs 1.9±0.01 days, p< 0.001). NVUGIB patients with COVID-19 patients were less likely to undergo EGD during the hospitalization (42.3% vs 60.2%, p< 0.001) and less likely to have EGD performed within 24 hours of presentation (20.7% vs 32.8%, OR 0.53, 0.46-0.61).
Discussion: Our nationally representative data suggests concurrent NVUGIB in patients with COVID-19 infection significantly increased mortality rates and healthcare utilization. The mortality rate in our study is lesser than the previously reported single center studies. Endoscopy was performed less frequently in COVID-19 patients with NVUGIB, along with a significant delay in time-to-EGD, although we could not provide evidence whether endoscopy was beneficial for these patients.
Disclosures:
Aizaz Khan indicated no relevant financial relationships.
Kamesh Gupta indicated no relevant financial relationships.
Victoria Caruso indicated no relevant financial relationships.
Aizaz Khan, MD1, Kamesh Gupta, MD2, Victoria Caruso, DO2. P0599 - COVID-19 in Non-Variceal Upper GI Bleeding: A National Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
