Sunday Poster Session
Category: GI Bleeding
P0613 - Mesenteric Variceal Bleed Presenting as Hemoperitoneum in New Onset Decompensated Liver Cirrhosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Edward Cay, DO
Spectrum Health Lakeland
St. Joseph, MI
Presenting Author(s)
Edward Cay, DO1, Thomas Birris, MD2
1Spectrum Health Lakeland, St. Joseph, MI; 2Great Lakes Gastroenterology, St. Joseph, MI
Introduction: Ectopic varices account for 5% of all variceal bleeds and a four fold increased risk of hemorrhage. In particular, mesenteric varices may cause hemoperitoneum that requires prompt diagnosis to avoid mortality.
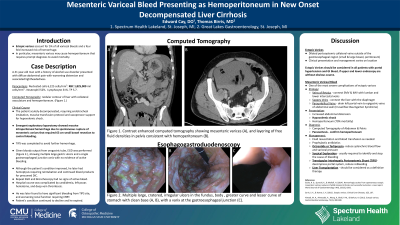
Case Description/Methods: A 41 year-old man with a history of alcohol use presented with diffuse abdominal pain with associated lightheadedness. There was no hematochezia, melena, or hematemesis. Diagnostic paracentesis was consistent with hemorrhagic ascites. Computed tomography revealed nodular contour of liver and hemoperitoneum. The patient then acutely decompensated, requiring endotracheal intubation, massive transfusion protocol and vasopressor support for hypovolemic shock. Emergent exploratory laparotomy showed massive intraperitoneal hemorrhage due to spontaneous rupture of mesenteric varices that required 63 cm small bowel resection to control bleeding.
TIPS was completed to avoid further hemorrhage. Given bloody output from orogastric tube, EGD was performed, showing multiple large gastric ulcers and a single gastroesophageal junction varix with no evidence of bleeding.
Although the patient’s condition improved, he later had hemoptysis requiring reintubation and continued blood products for presumed DIC. Repeat EGD and Bronchoscopy had no signs of active bleed. Hospital course was complicated by candidemia, left psoas hematoma, and deep vein thrombosis. He was later found to have significant bleeding from TIPS site, and worsening renal function requiring CRRT. Patient’s condition continued to decline and he expired.
Discussion: Ectopic varices are dilated portosystemic collateral veins outside of the gastroesophageal region, which includes small and large bowel as well as peritoneum.
Intraperitoneal varices in particular, such as the veins of Retzius, Sappey veins and paraumbilical veins, may rupture and lead to hemoperitoneum, which carries a 70% mortality. Most patients present with increased abdominal distension, hypovolemic shock and hemorrhagic ascites on paracentesis.
Initial management of mesenteric variceal bleed includes fluid resuscitation and blood transfusion as needed. Prophylactic antibiotics as well as octreotide or terlipressin have been utilized as well. Surgical exploration to identify and stop the cause of bleeding is usually required. While TIPS may decrease portal pressures, liver transplantation should be considered as a definitive therapy.

Disclosures:
Edward Cay, DO1, Thomas Birris, MD2. P0613 - Mesenteric Variceal Bleed Presenting as Hemoperitoneum in New Onset Decompensated Liver Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Spectrum Health Lakeland, St. Joseph, MI; 2Great Lakes Gastroenterology, St. Joseph, MI
Introduction: Ectopic varices account for 5% of all variceal bleeds and a four fold increased risk of hemorrhage. In particular, mesenteric varices may cause hemoperitoneum that requires prompt diagnosis to avoid mortality.
Case Description/Methods: A 41 year-old man with a history of alcohol use presented with diffuse abdominal pain with associated lightheadedness. There was no hematochezia, melena, or hematemesis. Diagnostic paracentesis was consistent with hemorrhagic ascites. Computed tomography revealed nodular contour of liver and hemoperitoneum. The patient then acutely decompensated, requiring endotracheal intubation, massive transfusion protocol and vasopressor support for hypovolemic shock. Emergent exploratory laparotomy showed massive intraperitoneal hemorrhage due to spontaneous rupture of mesenteric varices that required 63 cm small bowel resection to control bleeding.
TIPS was completed to avoid further hemorrhage. Given bloody output from orogastric tube, EGD was performed, showing multiple large gastric ulcers and a single gastroesophageal junction varix with no evidence of bleeding.
Although the patient’s condition improved, he later had hemoptysis requiring reintubation and continued blood products for presumed DIC. Repeat EGD and Bronchoscopy had no signs of active bleed. Hospital course was complicated by candidemia, left psoas hematoma, and deep vein thrombosis. He was later found to have significant bleeding from TIPS site, and worsening renal function requiring CRRT. Patient’s condition continued to decline and he expired.
Discussion: Ectopic varices are dilated portosystemic collateral veins outside of the gastroesophageal region, which includes small and large bowel as well as peritoneum.
Intraperitoneal varices in particular, such as the veins of Retzius, Sappey veins and paraumbilical veins, may rupture and lead to hemoperitoneum, which carries a 70% mortality. Most patients present with increased abdominal distension, hypovolemic shock and hemorrhagic ascites on paracentesis.
Initial management of mesenteric variceal bleed includes fluid resuscitation and blood transfusion as needed. Prophylactic antibiotics as well as octreotide or terlipressin have been utilized as well. Surgical exploration to identify and stop the cause of bleeding is usually required. While TIPS may decrease portal pressures, liver transplantation should be considered as a definitive therapy.

Figure: Contrast enhanced computed tomography showing mesenteric varices (A) and layering of fluid densities consistent with hemoperitoneum (B).
Disclosures:
Edward Cay indicated no relevant financial relationships.
Thomas Birris indicated no relevant financial relationships.
Edward Cay, DO1, Thomas Birris, MD2. P0613 - Mesenteric Variceal Bleed Presenting as Hemoperitoneum in New Onset Decompensated Liver Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
