Sunday Poster Session
Category: GI Bleeding
P0616 - Hematemesis Unveils a Hidden Culprit—Gastrointestinal AL Amyloidosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- AJ
Ali Jaan, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Ahmed Shehadah, MD1, Chengu Niu, MD1, Jason Gutman, MD1, Erik Olson, DO2, Karin Dunnigan, MD1, Patrick Okolo, MD, MPH, FACG1
1Rochester General Hospital, Rochester, NY; 2Rochester Regional Health, Rochester, NY
Introduction: Amyloidosis is caused by the extracellular deposition of abnormally folded proteins. Gastrointestinal (GI) amyloidosis usually affects the small intestine, followed by the stomach, esophagus, and colon. Common symptoms include abdominal pain, weight loss, diarrhea, and dysmotility. We report a case of AL amyloidosis presenting with acute hematemesis alongside chronic abdominal symptoms.
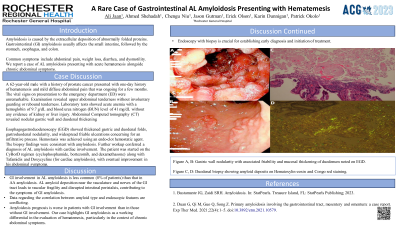
Case Description/Methods: A 62-year-old male with a history of prostate cancer presented with one day history of hematemesis and mild diffuse abdominal pain that was persistent for a few weeks. The vital signs on presentation to the emergency department (ED) were unremarkable. Examination revealed upper abdominal tenderness without involuntary guarding or rebound tenderness. Laboratory tests showed acute anemia with a hemoglobin of 9.7 g/dL and blood urea nitrogen (BUN) level of 41 mg/dL without any evidence of kidney or liver injury. Abdominal Computed tomography (CT) revealed nodular gastric wall and duodenal thickening. Esophagogastroduodenoscopy (EGD) showed thickened gastric and duodenal folds, gastroduodenal nodularity, and widespread friable ulcerations concerning for an infiltrative process. Hemostasis was achieved using an endo-clot hemostatic agent. The biopsy findings were consistent with amyloidosis. Further workup conferred a diagnosis of AL amyloidosis with cardiac involvement. The patient was started on the CyBorD regimen (cyclophosphamide, bortezomib, and dexamethasone) along with Tafamidis and Doxycycline (for cardiac amyloidosis), with eventual improvement in his abdominal symptoms.
Discussion: GI involvement in AL amyloidosis is less common (8% of patients) than that in AA amyloidosis. AL amyloid deposition near the vasculature and nerves of the GI tract leads to vascular fragility and disrupted intestinal peristalsis, contributing to the symptoms of GI amyloidosis. Data regarding the correlation between amyloid type and endoscopic features are conflicting. The treatment for GI manifestations of the underlying amyloidosis is mainly supportive. Our case highlights GI amyloidosis as a working differential in the evaluation of hematemesis, particularly in the context of chronic abdominal symptoms. Endoscopy with biopsy is crucial for establishing early diagnosis and initiation of treatment. Our case also supports the notion that AL amyloidosis commonly presents as mucosal fold thickening and polypoid protrusions.

Disclosures:
Ali Jaan, MD1, Ahmed Shehadah, MD1, Chengu Niu, MD1, Jason Gutman, MD1, Erik Olson, DO2, Karin Dunnigan, MD1, Patrick Okolo, MD, MPH, FACG1. P0616 - Hematemesis Unveils a Hidden Culprit—Gastrointestinal AL Amyloidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rochester Regional Health, Rochester, NY
Introduction: Amyloidosis is caused by the extracellular deposition of abnormally folded proteins. Gastrointestinal (GI) amyloidosis usually affects the small intestine, followed by the stomach, esophagus, and colon. Common symptoms include abdominal pain, weight loss, diarrhea, and dysmotility. We report a case of AL amyloidosis presenting with acute hematemesis alongside chronic abdominal symptoms.
Case Description/Methods: A 62-year-old male with a history of prostate cancer presented with one day history of hematemesis and mild diffuse abdominal pain that was persistent for a few weeks. The vital signs on presentation to the emergency department (ED) were unremarkable. Examination revealed upper abdominal tenderness without involuntary guarding or rebound tenderness. Laboratory tests showed acute anemia with a hemoglobin of 9.7 g/dL and blood urea nitrogen (BUN) level of 41 mg/dL without any evidence of kidney or liver injury. Abdominal Computed tomography (CT) revealed nodular gastric wall and duodenal thickening. Esophagogastroduodenoscopy (EGD) showed thickened gastric and duodenal folds, gastroduodenal nodularity, and widespread friable ulcerations concerning for an infiltrative process. Hemostasis was achieved using an endo-clot hemostatic agent. The biopsy findings were consistent with amyloidosis. Further workup conferred a diagnosis of AL amyloidosis with cardiac involvement. The patient was started on the CyBorD regimen (cyclophosphamide, bortezomib, and dexamethasone) along with Tafamidis and Doxycycline (for cardiac amyloidosis), with eventual improvement in his abdominal symptoms.
Discussion: GI involvement in AL amyloidosis is less common (8% of patients) than that in AA amyloidosis. AL amyloid deposition near the vasculature and nerves of the GI tract leads to vascular fragility and disrupted intestinal peristalsis, contributing to the symptoms of GI amyloidosis. Data regarding the correlation between amyloid type and endoscopic features are conflicting. The treatment for GI manifestations of the underlying amyloidosis is mainly supportive. Our case highlights GI amyloidosis as a working differential in the evaluation of hematemesis, particularly in the context of chronic abdominal symptoms. Endoscopy with biopsy is crucial for establishing early diagnosis and initiation of treatment. Our case also supports the notion that AL amyloidosis commonly presents as mucosal fold thickening and polypoid protrusions.

Figure: Figure A, B: Gastric wall nodularity with associated friability and mucosal thickening of duodenum noted on EGD. Figure C, D: Duodenal biopsy showing amyloid deposits on
Hematoxylin-eosin and Congo red staining.
Hematoxylin-eosin and Congo red staining.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Chengu Niu indicated no relevant financial relationships.
Jason Gutman indicated no relevant financial relationships.
Erik Olson indicated no relevant financial relationships.
Karin Dunnigan indicated no relevant financial relationships.
Patrick Okolo indicated no relevant financial relationships.
Ali Jaan, MD1, Ahmed Shehadah, MD1, Chengu Niu, MD1, Jason Gutman, MD1, Erik Olson, DO2, Karin Dunnigan, MD1, Patrick Okolo, MD, MPH, FACG1. P0616 - Hematemesis Unveils a Hidden Culprit—Gastrointestinal AL Amyloidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
