Sunday Poster Session
Category: GI Bleeding
P0624 - Heyde Syndrome Associated With Recurrent GI Bleeding, Severe Aortic Stenosis & Acquired Von Willebrand Deficiency
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- GS
Guneet Sidhu, MD
University of North Dakota School of Medicine
Fargo, ND
Presenting Author(s)
Guneet Sidhu, MD1, John T. Bassett, MD2
1University of North Dakota School of Medicine, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Heyde syndrome is described as a triad of gastrointestinal atrial venous malformations, aortic stenosis and acquired von Willebrand's deficiency.
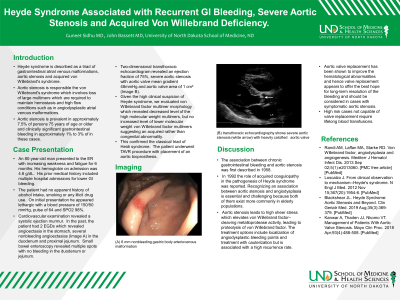
Case Description/Methods: An 80-year-old man presented to the ER with increasing weakness and fatigue for 6 months. Hemoglobin on admission was 4.6 g/dL. His prior medical history included multiple hospital admissions for lower GI bleeding. No apparent history of alcohol intake, smoking or any illicit drug use. On initial presentation he appeared lethargic with a BP of 150/50 mmHg, HR 64 and SPO2 98%. Cardiovascular examination revealed a systolic ejection murmur. In the past, the patient had 2 EGDs which revealed several nonbleeding angioectasias (Image A) in the duodenum and proximal jejunum. Small bowel enteroscopy revealed multiple spots with no bleeding in the duodenum or jejenum. Two-dimensional transthoracic echocardiogram revealed an ejection fraction of 75%, severe aortic stenosis with aortic valve mean gradient 48mmHg and aortic valve area of 1 cm² (Image B). Given the high clinical suspicion of Heyde syndrome, we evaluated von Willebrand factor multimer morphology which revealed decreased level of the high molecular weight multimers, but no increased level of lower molecular weight von Willebrand factor multimers suggesting an acquired rather than congenital abnormality. This confirmed the classical triad of Heidi syndrome. The patient underwent TAVR procedure with placement of an aortic bioprosthesis.
Discussion: The association between chronic gastrointestinal bleeding and aortic stenosis was first described in 1958. In 1992 the role of acquired coagulopathy in the pathogenesis of Heyde syndrome was reported. Recognizing an association between aortic stenosis and angiodysplasia is essential and challenging because both of them exist more commonly in elderly populations. Aortic stenosis leads to high sheer stress which elevates von Willebrand factor–cleaving metalloprotease activity, leading to proteolysis of von Willebrand factor. The treatment options include localization of angiodysplastic bleeding points and treatment with cauterization but is associated with a high recurrence rate. Aortic valve replacement has been shown to improve the hematological abnormalities and hence valve replacement appears to offer the best hope for long-term resolution of the bleeding and should be considered in cases with symptomatic aortic stenosis. High risk cases not capable of valve replacement require lifelong blood transfusions.

Disclosures:
Guneet Sidhu, MD1, John T. Bassett, MD2. P0624 - Heyde Syndrome Associated With Recurrent GI Bleeding, Severe Aortic Stenosis & Acquired Von Willebrand Deficiency, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of North Dakota School of Medicine, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Heyde syndrome is described as a triad of gastrointestinal atrial venous malformations, aortic stenosis and acquired von Willebrand's deficiency.
Case Description/Methods: An 80-year-old man presented to the ER with increasing weakness and fatigue for 6 months. Hemoglobin on admission was 4.6 g/dL. His prior medical history included multiple hospital admissions for lower GI bleeding. No apparent history of alcohol intake, smoking or any illicit drug use. On initial presentation he appeared lethargic with a BP of 150/50 mmHg, HR 64 and SPO2 98%. Cardiovascular examination revealed a systolic ejection murmur. In the past, the patient had 2 EGDs which revealed several nonbleeding angioectasias (Image A) in the duodenum and proximal jejunum. Small bowel enteroscopy revealed multiple spots with no bleeding in the duodenum or jejenum. Two-dimensional transthoracic echocardiogram revealed an ejection fraction of 75%, severe aortic stenosis with aortic valve mean gradient 48mmHg and aortic valve area of 1 cm² (Image B). Given the high clinical suspicion of Heyde syndrome, we evaluated von Willebrand factor multimer morphology which revealed decreased level of the high molecular weight multimers, but no increased level of lower molecular weight von Willebrand factor multimers suggesting an acquired rather than congenital abnormality. This confirmed the classical triad of Heidi syndrome. The patient underwent TAVR procedure with placement of an aortic bioprosthesis.
Discussion: The association between chronic gastrointestinal bleeding and aortic stenosis was first described in 1958. In 1992 the role of acquired coagulopathy in the pathogenesis of Heyde syndrome was reported. Recognizing an association between aortic stenosis and angiodysplasia is essential and challenging because both of them exist more commonly in elderly populations. Aortic stenosis leads to high sheer stress which elevates von Willebrand factor–cleaving metalloprotease activity, leading to proteolysis of von Willebrand factor. The treatment options include localization of angiodysplastic bleeding points and treatment with cauterization but is associated with a high recurrence rate. Aortic valve replacement has been shown to improve the hematological abnormalities and hence valve replacement appears to offer the best hope for long-term resolution of the bleeding and should be considered in cases with symptomatic aortic stenosis. High risk cases not capable of valve replacement require lifelong blood transfusions.

Figure: (A) 6 mm nonbleeding gastric body arteriovenous malformation
(B) transthoracic echocardiography shows severe aortic stenosis (white arrow) with heavily calcified aortic valve
(B) transthoracic echocardiography shows severe aortic stenosis (white arrow) with heavily calcified aortic valve
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Guneet Sidhu, MD1, John T. Bassett, MD2. P0624 - Heyde Syndrome Associated With Recurrent GI Bleeding, Severe Aortic Stenosis & Acquired Von Willebrand Deficiency, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
