Sunday Poster Session
Category: GI Bleeding
P0626 - A Missed Case of Hereditary Hemorrhagic Telangiectasia
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Het Patel, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Het Patel, DO1, Janak Bahirwani, MD2, Naomi Reddy-Patel, MD3, Yecheskel Schneider, MD1
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Bethlehem, PA; 3St. Luke's University Health Network, Bethlehem, PA
Introduction: Hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu syndrome, is a rare autosomal dominant genetic mutation that causes telangiectasias, arteriovenous malformations (AVMs), and mucocutaneous lesion in multiple organs including the brain, lung, liver, skin, mucous membranes, and GI tract. AVMs may present throughout the alimentary canal and my present with recurrent overt or occult GI bleed.
Case Description/Methods: A 65-year-old male presented to the hospital with 3-day history of melena and symptomatic anemia. The patient has known history of recurrent GI bleed previously found to have numerous AVMs in the stomach, duodenum, and colon. The patient was hemodynamically stable, however labs revealed hemoglobin of 8.4g/dL. Upper endoscopy was performed the following day which showed multiple AVMs in the stomach, duodenum, and jejunum treated with argon plasma coagulation (APC) and was subsequently discharged with a proton pump inhibitor and octreotide. Outpatient capsule endoscopy showed small non-bleeding erosions and AVMs from the duodenum to the distal ileum. Further investigation revealed history of recurrent spontaneous epistaxis, recurrent epistaxis and GI bleed in his siblings, and stroke in father and sister. With this the patient met the Curacao Criteria and genetic testing identified heterozygous deletion of exon 1 to 4 in the ACVRL1 gene confirming the diagnosis of hereditary hemorrhagic telangiectasia. He was followed up with brain and abdomen MRI which did not reveal any lesions.
Discussion: The prevalence of HHT is 1 in 5000, and it most commonly presents with spontaneous epistaxis occurring in 90-95% of patients and 40-50% of patients will develop GI bleed.1 Many patients such as the patient discussed, do not develop the clinical manifestations that clue prompt diagnosis of HHT and may result in delayed or missed diagnosis. This patient had multiple endoscopies which revealed numerous AVMs for the past 3 years without established or even suspected diagnosis which delays further management which includes screening pulmonary, cerebral, and hepatic AVMs and recommend genetic screening for at risk family members. Multiple AVMs on endoscopy should raise suspicion for HHT and prompt further investigation of history of epistaxis and family history regardless of age or overt physical findings to allow timely diagnosis and screening.
Ferri F, Heather F. Hereditary Hemorrhagic Telangiectasia . Clinical Key. Published January 1, 2023.

Disclosures:
Het Patel, DO1, Janak Bahirwani, MD2, Naomi Reddy-Patel, MD3, Yecheskel Schneider, MD1. P0626 - A Missed Case of Hereditary Hemorrhagic Telangiectasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Bethlehem, PA; 3St. Luke's University Health Network, Bethlehem, PA
Introduction: Hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu syndrome, is a rare autosomal dominant genetic mutation that causes telangiectasias, arteriovenous malformations (AVMs), and mucocutaneous lesion in multiple organs including the brain, lung, liver, skin, mucous membranes, and GI tract. AVMs may present throughout the alimentary canal and my present with recurrent overt or occult GI bleed.
Case Description/Methods: A 65-year-old male presented to the hospital with 3-day history of melena and symptomatic anemia. The patient has known history of recurrent GI bleed previously found to have numerous AVMs in the stomach, duodenum, and colon. The patient was hemodynamically stable, however labs revealed hemoglobin of 8.4g/dL. Upper endoscopy was performed the following day which showed multiple AVMs in the stomach, duodenum, and jejunum treated with argon plasma coagulation (APC) and was subsequently discharged with a proton pump inhibitor and octreotide. Outpatient capsule endoscopy showed small non-bleeding erosions and AVMs from the duodenum to the distal ileum. Further investigation revealed history of recurrent spontaneous epistaxis, recurrent epistaxis and GI bleed in his siblings, and stroke in father and sister. With this the patient met the Curacao Criteria and genetic testing identified heterozygous deletion of exon 1 to 4 in the ACVRL1 gene confirming the diagnosis of hereditary hemorrhagic telangiectasia. He was followed up with brain and abdomen MRI which did not reveal any lesions.
Discussion: The prevalence of HHT is 1 in 5000, and it most commonly presents with spontaneous epistaxis occurring in 90-95% of patients and 40-50% of patients will develop GI bleed.1 Many patients such as the patient discussed, do not develop the clinical manifestations that clue prompt diagnosis of HHT and may result in delayed or missed diagnosis. This patient had multiple endoscopies which revealed numerous AVMs for the past 3 years without established or even suspected diagnosis which delays further management which includes screening pulmonary, cerebral, and hepatic AVMs and recommend genetic screening for at risk family members. Multiple AVMs on endoscopy should raise suspicion for HHT and prompt further investigation of history of epistaxis and family history regardless of age or overt physical findings to allow timely diagnosis and screening.
Ferri F, Heather F. Hereditary Hemorrhagic Telangiectasia . Clinical Key. Published January 1, 2023.

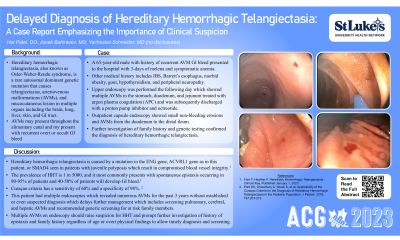
Figure: Bleeding arteriovenous malformation (AVM) in a patient with hereditary hemorrhagic telangiectasia (HHT).
Disclosures:
Het Patel indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Naomi Reddy-Patel indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Het Patel, DO1, Janak Bahirwani, MD2, Naomi Reddy-Patel, MD3, Yecheskel Schneider, MD1. P0626 - A Missed Case of Hereditary Hemorrhagic Telangiectasia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
