Sunday Poster Session
Category: GI Bleeding
P0627 - Gastrointestinal Vasculitis in a Case of Adult Dermatomyositis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Susie Min, MD
University of Cincinnati College of Medicine
Ann Arbor, MI
Presenting Author(s)
Susie Min, MD1, Debra Yen, MD2, Gail Bongiovanni, MD2
1University of Cincinnati College of Medicine, Cincinnati, OH; 2University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Dermatomyositis (DM) is an inflammatory disease of the muscles and skin. Gastrointestinal (GI) involvement can be seen in over 50% of cases, with dysphagia being the most well recognized.1,2 However, others describe rare cases of ulcers, vasculopathy, and perforation.3–6 We present a case of newly diagnosed DM with hematemesis from duodenal ulcers from leukocytoclastic vasculitis, which healed with DM treatment.
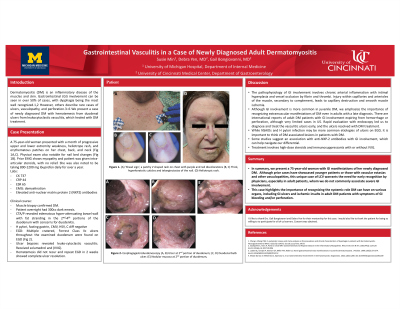
Case Description/Methods: A 75-year-old woman presented with a month of progressive extremity weakness, heliotrope rash, and erythematous patches on her chest, back, and neck. Labs were notable for creatine kinase of 737, CRP 44, ESR 65, demyelination on EMG, and elevated anti-nuclear matrix protein 2 (NXP2) antibodies. Thigh muscle biopsy results confirmed DM. She then had sudden hematemesis. Multiple cratered, Forrest Class IIc ulcers throughout the examined duodenum were found on EGD (Fig 1). Ulcer biopsies revealed leukocytoclastic vasculitis. She was treated with solumedrol and intravenous immunoglobulin (IVIG). Hematemesis did not recur, and repeat EGD in 2 weeks showed complete ulcer resolution.
Discussion: We emphasize the importance of recognizing extramuscular DM manifestations, including the GI tract, even in adult patients with a late diagnosis. Severe GI involvement, mostly described in juvenile DM (JDM) cases, can also occur in adults.7–10 Indeed, international reports of adult DM patients with GI involvement expired from hemorrhage or perforation.11 In our case, rapid evaluation with endoscopy led us to diagnose and treat the vasculitic ulcers early, and the ulcers resolved with DM treatment.
Gastrointestinal vasculitis is a rare presentation of DM,2 and studies suggest an association with NXP-2 antibodies and GI perforation in JDM.12 The pathophysiology of GI involvement involves chronic arterial inflammation with intimal hyperplasia and vessel occlusion by fibrin and thrombi. Injury within capillaries and arterioles of the muscle, secondary to complement, leads to capillary destruction and smooth muscle ischemia.9 DM patients with GI involvement often present with classic DM signs,4 including Gottron’s papules, heliotrope rash, and shawl sign. Treatment involves high-dose steroids and immunosuppressants with or without IVIG. This case highlights the importance of recognizing the systemic role DM can have on various organs, including GI ulcers and ischemic insults in adult DM patients with symptoms of GI bleeding and/or perforation.

Disclosures:
Susie Min, MD1, Debra Yen, MD2, Gail Bongiovanni, MD2. P0627 - Gastrointestinal Vasculitis in a Case of Adult Dermatomyositis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Cincinnati College of Medicine, Cincinnati, OH; 2University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Dermatomyositis (DM) is an inflammatory disease of the muscles and skin. Gastrointestinal (GI) involvement can be seen in over 50% of cases, with dysphagia being the most well recognized.1,2 However, others describe rare cases of ulcers, vasculopathy, and perforation.3–6 We present a case of newly diagnosed DM with hematemesis from duodenal ulcers from leukocytoclastic vasculitis, which healed with DM treatment.
Case Description/Methods: A 75-year-old woman presented with a month of progressive extremity weakness, heliotrope rash, and erythematous patches on her chest, back, and neck. Labs were notable for creatine kinase of 737, CRP 44, ESR 65, demyelination on EMG, and elevated anti-nuclear matrix protein 2 (NXP2) antibodies. Thigh muscle biopsy results confirmed DM. She then had sudden hematemesis. Multiple cratered, Forrest Class IIc ulcers throughout the examined duodenum were found on EGD (Fig 1). Ulcer biopsies revealed leukocytoclastic vasculitis. She was treated with solumedrol and intravenous immunoglobulin (IVIG). Hematemesis did not recur, and repeat EGD in 2 weeks showed complete ulcer resolution.
Discussion: We emphasize the importance of recognizing extramuscular DM manifestations, including the GI tract, even in adult patients with a late diagnosis. Severe GI involvement, mostly described in juvenile DM (JDM) cases, can also occur in adults.7–10 Indeed, international reports of adult DM patients with GI involvement expired from hemorrhage or perforation.11 In our case, rapid evaluation with endoscopy led us to diagnose and treat the vasculitic ulcers early, and the ulcers resolved with DM treatment.
Gastrointestinal vasculitis is a rare presentation of DM,2 and studies suggest an association with NXP-2 antibodies and GI perforation in JDM.12 The pathophysiology of GI involvement involves chronic arterial inflammation with intimal hyperplasia and vessel occlusion by fibrin and thrombi. Injury within capillaries and arterioles of the muscle, secondary to complement, leads to capillary destruction and smooth muscle ischemia.9 DM patients with GI involvement often present with classic DM signs,4 including Gottron’s papules, heliotrope rash, and shawl sign. Treatment involves high-dose steroids and immunosuppressants with or without IVIG. This case highlights the importance of recognizing the systemic role DM can have on various organs, including GI ulcers and ischemic insults in adult DM patients with symptoms of GI bleeding and/or perforation.

Figure: Figure 1- Endoscopy of the duodenum at time of hematemesis showing ulcers with pigmented spots.
Disclosures:
Susie Min indicated no relevant financial relationships.
Debra Yen indicated no relevant financial relationships.
Gail Bongiovanni indicated no relevant financial relationships.
Susie Min, MD1, Debra Yen, MD2, Gail Bongiovanni, MD2. P0627 - Gastrointestinal Vasculitis in a Case of Adult Dermatomyositis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
