Sunday Poster Session
Category: GI Bleeding
P0629 - Gastric Plexiform Fibromyxoma: A Rare Cause of Recurrent Upper GI Bleeding
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ahmad Al-Dwairy, MBBS
MedStar Georgetown Washington Hospital Center
Washington, DC
Presenting Author(s)
Award: Presidential Poster Award
Ahmad Al-Dwairy, MBBS1, Ajay Jassal, MS2, Jessica Rosenberg, MD3, Stanley Pietrak III, MD4
1MedStar Georgetown Washington Hospital Center, Washington, DC; 2Georgetown University, Washington, DC; 3MedStar Georgetown University Hospital, Washington, DC; 4MedtStar Georgetown University Hospital, Washington, DC
Introduction: Gastric plexiform fibromyxoma (PF) is a rare, benign neoplasm most often found in the gastric antrum. Presentation ranges from incidental to recurrent gastrointestinal (GI) bleeding. Differentiation from other tumors, specifically gastrointestinal stromal tumors (GIST), is essential for management.
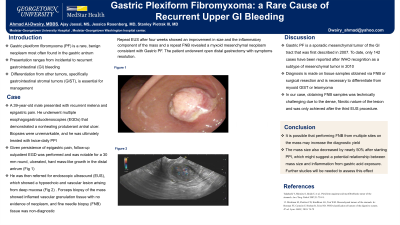
Case Description/Methods: A 39-year-old male presented with recurrent melena and epigastric pain. He underwent multiple esophagogastroduodenoscopies (EGDs) that demonstrated a nonhealing protuberant antral ulcer. Biopsies were unremarkable, and he was ultimately treated with twice-daily PPI. Although his melena stopped, he continued to have epigastric pain. A follow-up outpatient EGD was performed and was notable for a 30 mm round, ulcerated, hard mass-like growth in the distal antrum (Fig 1).
He was then referred for endoscopic ultrasound (EUS), which showed a hypoechoic and vascular lesion arising from deep mucosa. Forceps biopsy of the mass showed inflamed vascular granulation tissue with no evidence of neoplasm, and fine needle biopsy (FNB) tissue was non-diagnostic
Repeat EUS after four weeks showed a persistent but less inflamed mass in the antrum. A repeat FNB showed benign reactive glandular epithelium. The patient continued to have epigastric pain, and a repeat EUS after another four weeks was performed. There was an improvement in the size and inflammatory component of the mass, and a repeat FNB revealed a myxoid mesenchymal neoplasm consistent with gastric PF. The patient underwent open distal gastrectomy with symptoms resolution.
Discussion: Gastric PF is a sporadic mesenchymal tumor of the GI tract that was first described in 2007. To date, only 142 cases have been reported after WHO recognition as a subtype of mesenchymal tumor in 2010
Diagnosis is made on tissue samples obtained via FNB or surgical resection and is necessary to differentiate from myxoid GIST or leiomyoma. CT and MRI can help determine/confirm size and location, but PF is not known to invade structures outside of the stomach or metastasize
In our case, obtaining FNB samples was technically challenging due to the dense, fibrotic nature of the lesion and was only achieved after the third EUS procedure. It is possible that performing FNB from multiple sites on the mass may increase the diagnostic yield. The mass size also decreased by nearly 50% after starting PPI, which might suggest a potential relationship between mass size and inflammation from gastric acid exposure. Further studies will be needed to assess this effect.

Disclosures:
Ahmad Al-Dwairy, MBBS1, Ajay Jassal, MS2, Jessica Rosenberg, MD3, Stanley Pietrak III, MD4. P0629 - Gastric Plexiform Fibromyxoma: A Rare Cause of Recurrent Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Ahmad Al-Dwairy, MBBS1, Ajay Jassal, MS2, Jessica Rosenberg, MD3, Stanley Pietrak III, MD4
1MedStar Georgetown Washington Hospital Center, Washington, DC; 2Georgetown University, Washington, DC; 3MedStar Georgetown University Hospital, Washington, DC; 4MedtStar Georgetown University Hospital, Washington, DC
Introduction: Gastric plexiform fibromyxoma (PF) is a rare, benign neoplasm most often found in the gastric antrum. Presentation ranges from incidental to recurrent gastrointestinal (GI) bleeding. Differentiation from other tumors, specifically gastrointestinal stromal tumors (GIST), is essential for management.
Case Description/Methods: A 39-year-old male presented with recurrent melena and epigastric pain. He underwent multiple esophagogastroduodenoscopies (EGDs) that demonstrated a nonhealing protuberant antral ulcer. Biopsies were unremarkable, and he was ultimately treated with twice-daily PPI. Although his melena stopped, he continued to have epigastric pain. A follow-up outpatient EGD was performed and was notable for a 30 mm round, ulcerated, hard mass-like growth in the distal antrum (Fig 1).
He was then referred for endoscopic ultrasound (EUS), which showed a hypoechoic and vascular lesion arising from deep mucosa. Forceps biopsy of the mass showed inflamed vascular granulation tissue with no evidence of neoplasm, and fine needle biopsy (FNB) tissue was non-diagnostic
Repeat EUS after four weeks showed a persistent but less inflamed mass in the antrum. A repeat FNB showed benign reactive glandular epithelium. The patient continued to have epigastric pain, and a repeat EUS after another four weeks was performed. There was an improvement in the size and inflammatory component of the mass, and a repeat FNB revealed a myxoid mesenchymal neoplasm consistent with gastric PF. The patient underwent open distal gastrectomy with symptoms resolution.
Discussion: Gastric PF is a sporadic mesenchymal tumor of the GI tract that was first described in 2007. To date, only 142 cases have been reported after WHO recognition as a subtype of mesenchymal tumor in 2010
Diagnosis is made on tissue samples obtained via FNB or surgical resection and is necessary to differentiate from myxoid GIST or leiomyoma. CT and MRI can help determine/confirm size and location, but PF is not known to invade structures outside of the stomach or metastasize
In our case, obtaining FNB samples was technically challenging due to the dense, fibrotic nature of the lesion and was only achieved after the third EUS procedure. It is possible that performing FNB from multiple sites on the mass may increase the diagnostic yield. The mass size also decreased by nearly 50% after starting PPI, which might suggest a potential relationship between mass size and inflammation from gastric acid exposure. Further studies will be needed to assess this effect.

Figure: 30 mm round, ulcerated, hard mass-like growth in the distal antrum with hypoechoic and vascular lesion arising from deep mucosa with no surrounding lymphadenopathy
Disclosures:
Ahmad Al-Dwairy indicated no relevant financial relationships.
Ajay Jassal indicated no relevant financial relationships.
Jessica Rosenberg indicated no relevant financial relationships.
Stanley Pietrak III indicated no relevant financial relationships.
Ahmad Al-Dwairy, MBBS1, Ajay Jassal, MS2, Jessica Rosenberg, MD3, Stanley Pietrak III, MD4. P0629 - Gastric Plexiform Fibromyxoma: A Rare Cause of Recurrent Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


