Sunday Poster Session
Category: GI Bleeding
P0630 - Pancreatic Pseudoaneurysm: A Rare Cause of Upper GI Bleed
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DA
Dominic Amakye, MD
Piedmont Athens Regional Medical Center
Athens, GA
Presenting Author(s)
Dominic Amakye, MD, Isaac Opoku, MD, Raissa Nana, MD, Elizabeth Soladoye, MD, Amal Naji, MD, Kikelomo Olaosebikan, MD
Piedmont Athens Regional Medical Center, Athens, GA
Introduction: Pancreatic pseudoaneurysm (PSA) is a rare clinical entity that may occur as a late complication of pancreatitis, pancreaticobiliary surgery or following trauma to the abdomen. It is reported that about 10% of patients with pancreatitis may develop a PSA. PSA is mostly asymptomatic but can suddenly evolve into a potentially life-threatening gastrointestinal bleed with poor outcomes hence the need for prompt intervention when incidentally identified. We report an interesting case of a young adult with recurrent pancreatitis who presented with an upper GI bleed due to PSA that was successfully treated with embolization.
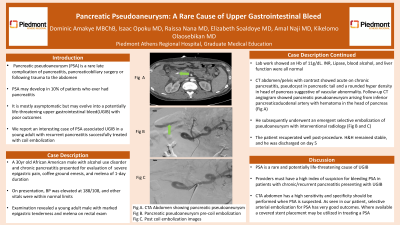
Case Description/Methods: A 30yr old African American male with a history of alcohol use disorder and chronic pancreatitis presented to the emergency department with severe epigastric pain, coffee ground emesis, and melena of 1-day duration. On presentation, BP was elevated at 188/108, and other vitals were within normal limits. Examination revealed a young adult male with marked epigastric tenderness and melena on rectal exam. Lab work showed an Hb of 11g/dL. Lipase, blood alcohol, and liver function were all normal. A CT abdomen/pelvis with contrast showed acute on chronic pancreatitis, a pseudocyst in the pancreatic tail and a rounded hyperdensity in the head of the pancreas suggestive of a vascular abnormality. A follow-up CT angiogram of the abdomen showed a pancreatic pseudoaneurysm possibly from the inferior pancreaticoduodenal artery with hematoma in the head of the pancreas ( figure A). The patient subsequently underwent an emergent selective embolization of pseudoaneurysm with interventional radiology (Figures B and C). He recuperated well post-procedure with resolution of abdominal pain. H&H remained stable, and he was discharged after 5 days to follow up with gastroenterology outpatient.
Discussion: PSA is a rare cause of upper GI bleed and is potentially life-threatening if not promptly identified and treated. In patients with a strong history of recurrent pancreatitis or chronic pancreatitis who present with an upper GI bleed providers must have a high index of suspicion for bleeding PSA. In instances where a PSA bleed is suspected a prompt CTA angiogram should be performed since this has a high sensitivity and specificity. If an aneurysm is identified patients can undergo selective arterial embolization with good outcomes as illustrated in our patient. There is also the role of covered stent placement in treating a PSA if this is readily available.

Disclosures:
Dominic Amakye, MD, Isaac Opoku, MD, Raissa Nana, MD, Elizabeth Soladoye, MD, Amal Naji, MD, Kikelomo Olaosebikan, MD. P0630 - Pancreatic Pseudoaneurysm: A Rare Cause of Upper GI Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Piedmont Athens Regional Medical Center, Athens, GA
Introduction: Pancreatic pseudoaneurysm (PSA) is a rare clinical entity that may occur as a late complication of pancreatitis, pancreaticobiliary surgery or following trauma to the abdomen. It is reported that about 10% of patients with pancreatitis may develop a PSA. PSA is mostly asymptomatic but can suddenly evolve into a potentially life-threatening gastrointestinal bleed with poor outcomes hence the need for prompt intervention when incidentally identified. We report an interesting case of a young adult with recurrent pancreatitis who presented with an upper GI bleed due to PSA that was successfully treated with embolization.
Case Description/Methods: A 30yr old African American male with a history of alcohol use disorder and chronic pancreatitis presented to the emergency department with severe epigastric pain, coffee ground emesis, and melena of 1-day duration. On presentation, BP was elevated at 188/108, and other vitals were within normal limits. Examination revealed a young adult male with marked epigastric tenderness and melena on rectal exam. Lab work showed an Hb of 11g/dL. Lipase, blood alcohol, and liver function were all normal. A CT abdomen/pelvis with contrast showed acute on chronic pancreatitis, a pseudocyst in the pancreatic tail and a rounded hyperdensity in the head of the pancreas suggestive of a vascular abnormality. A follow-up CT angiogram of the abdomen showed a pancreatic pseudoaneurysm possibly from the inferior pancreaticoduodenal artery with hematoma in the head of the pancreas ( figure A). The patient subsequently underwent an emergent selective embolization of pseudoaneurysm with interventional radiology (Figures B and C). He recuperated well post-procedure with resolution of abdominal pain. H&H remained stable, and he was discharged after 5 days to follow up with gastroenterology outpatient.
Discussion: PSA is a rare cause of upper GI bleed and is potentially life-threatening if not promptly identified and treated. In patients with a strong history of recurrent pancreatitis or chronic pancreatitis who present with an upper GI bleed providers must have a high index of suspicion for bleeding PSA. In instances where a PSA bleed is suspected a prompt CTA angiogram should be performed since this has a high sensitivity and specificity. If an aneurysm is identified patients can undergo selective arterial embolization with good outcomes as illustrated in our patient. There is also the role of covered stent placement in treating a PSA if this is readily available.

Figure: A; CT angiogram of the abdomen showing pancreatic pseudoaneurysm bleed
B: Pancreatic pseudoaneurysm pre-selective arterial coil embolization
C: Post embolization image
B: Pancreatic pseudoaneurysm pre-selective arterial coil embolization
C: Post embolization image
Disclosures:
Dominic Amakye indicated no relevant financial relationships.
Isaac Opoku indicated no relevant financial relationships.
Raissa Nana indicated no relevant financial relationships.
Elizabeth Soladoye indicated no relevant financial relationships.
Amal Naji indicated no relevant financial relationships.
Kikelomo Olaosebikan indicated no relevant financial relationships.
Dominic Amakye, MD, Isaac Opoku, MD, Raissa Nana, MD, Elizabeth Soladoye, MD, Amal Naji, MD, Kikelomo Olaosebikan, MD. P0630 - Pancreatic Pseudoaneurysm: A Rare Cause of Upper GI Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
