Sunday Poster Session
Category: GI Bleeding
P0632 - Intestinal Phlebectasias: An Underestimated Cause of Overt Gastrointestinal Bleeding
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Karelys Burgos Irizarry, MD
University of Puerto Rico Medical Sciences Campus
San Juan, Puerto Rico
Presenting Author(s)
Karelys Burgos-Irizarry, MD1, Yue-Sai Jao-Ayala, MD1, Paola Laracuente-Román, MD2, José Muñoz-Acaba, MD3, Loscar Santiago-Rivera, MD3, Joham Senior-Marino, MD2, Jesús Rivera-Román, BS4
1University of Puerto Rico Medical Sciences Campus, San Juan, Puerto Rico; 2University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 3San Juan, Puerto Rico; 4University of Puerto Rico, Río Piedras Campus, San Juan, Puerto Rico
Introduction: Intestinal phlebectasias are a rare vascular abnormality characterized by dilated tortuous veins with bluish-red macroscopic appearance. Most commonly involve the jejunum and unusually may lead to severe overt gastrointestinal bleeding (GI). Management options include sclerotherapy and surgery, nonetheless due to their multiplicity and location they represent a diagnostic and therapeutic challenge. We present the case of life-threatening bleeding secondary to jejunal phlebectasias.
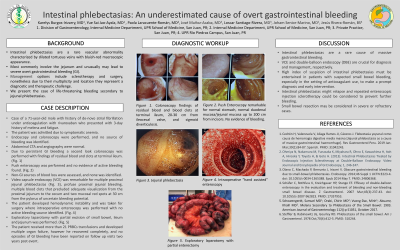
Case Description/Methods: Case of a 71-year-old male with history of de-novo atrial fibrillation under anticoagulation with ribaroxaban who presented with 3-day history of melena and fatigue. The patient was admitted due to symptomatic anemia. Endoscopy was performed and no source of bleeding was identified. Colonoscopy was remarkable for bright red blood and blood clots at terminal ileum and right colon. Abdominal CTA and angiography were normal. Due to persistent GI bleeding a second look colonoscopy was performed with findings of residual blood and clots at terminal ileum. Push enteroscopy was performed and no evidence of active bleeding found. Non-GI sources of blood loss were assessed, and none was identified. Video capsule endoscopy (VCE) was remarkable for multiple proximal jejunal phlebectasias (Fig. 1), profuse proximal jejunal bleeding, multiple blood clots that precluded adequate visualization from proximal jejunum to cecum and two mucosal red spots at 30 cm from the pylorus of uncertain bleeding potential. The patient developed hemodynamic instability and was taken for surgery where intraoperative enteroscopy was performed with no active bleeding source identified. Exploratory laparotomy with partial excision of small bowel, ileum and jejunum was performed. The patient received more than 21 PRBCs transfusions and developed multiple organ failure, however he recovered completely, and no episodes of GI bleeding have been reported on follow up visits two years post event.
Discussion: Intestinal phlebectasias are a rare cause of massive gastrointestinal bleeding. VCE and double-balloon endoscopy (DBE) are crucial for diagnosis and management respectively. High index of suspicion of intestinal phlebectasias must be entertained in patients with suspected small bowel bleeding, especially in the setting of anticoagulant use, to make a prompt diagnosis and early intervention. Intestinal phlebectasias might relapse and repeated enteroscopic injection sclerotherapy could be considered to prevent further bleeding.

Disclosures:
Karelys Burgos-Irizarry, MD1, Yue-Sai Jao-Ayala, MD1, Paola Laracuente-Román, MD2, José Muñoz-Acaba, MD3, Loscar Santiago-Rivera, MD3, Joham Senior-Marino, MD2, Jesús Rivera-Román, BS4. P0632 - Intestinal Phlebectasias: An Underestimated Cause of Overt Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Puerto Rico Medical Sciences Campus, San Juan, Puerto Rico; 2University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 3San Juan, Puerto Rico; 4University of Puerto Rico, Río Piedras Campus, San Juan, Puerto Rico
Introduction: Intestinal phlebectasias are a rare vascular abnormality characterized by dilated tortuous veins with bluish-red macroscopic appearance. Most commonly involve the jejunum and unusually may lead to severe overt gastrointestinal bleeding (GI). Management options include sclerotherapy and surgery, nonetheless due to their multiplicity and location they represent a diagnostic and therapeutic challenge. We present the case of life-threatening bleeding secondary to jejunal phlebectasias.
Case Description/Methods: Case of a 71-year-old male with history of de-novo atrial fibrillation under anticoagulation with ribaroxaban who presented with 3-day history of melena and fatigue. The patient was admitted due to symptomatic anemia. Endoscopy was performed and no source of bleeding was identified. Colonoscopy was remarkable for bright red blood and blood clots at terminal ileum and right colon. Abdominal CTA and angiography were normal. Due to persistent GI bleeding a second look colonoscopy was performed with findings of residual blood and clots at terminal ileum. Push enteroscopy was performed and no evidence of active bleeding found. Non-GI sources of blood loss were assessed, and none was identified. Video capsule endoscopy (VCE) was remarkable for multiple proximal jejunal phlebectasias (Fig. 1), profuse proximal jejunal bleeding, multiple blood clots that precluded adequate visualization from proximal jejunum to cecum and two mucosal red spots at 30 cm from the pylorus of uncertain bleeding potential. The patient developed hemodynamic instability and was taken for surgery where intraoperative enteroscopy was performed with no active bleeding source identified. Exploratory laparotomy with partial excision of small bowel, ileum and jejunum was performed. The patient received more than 21 PRBCs transfusions and developed multiple organ failure, however he recovered completely, and no episodes of GI bleeding have been reported on follow up visits two years post event.
Discussion: Intestinal phlebectasias are a rare cause of massive gastrointestinal bleeding. VCE and double-balloon endoscopy (DBE) are crucial for diagnosis and management respectively. High index of suspicion of intestinal phlebectasias must be entertained in patients with suspected small bowel bleeding, especially in the setting of anticoagulant use, to make a prompt diagnosis and early intervention. Intestinal phlebectasias might relapse and repeated enteroscopic injection sclerotherapy could be considered to prevent further bleeding.

Figure: Figure 1. Jejunal phlebectasias
Disclosures:
Karelys Burgos-Irizarry indicated no relevant financial relationships.
Yue-Sai Jao-Ayala indicated no relevant financial relationships.
Paola Laracuente-Román indicated no relevant financial relationships.
José Muñoz-Acaba: Sanofi – Advisory Committee/Board Member.
Loscar Santiago-Rivera indicated no relevant financial relationships.
Joham Senior-Marino: Sanofi – Advisory Committee/Board Member, Speakers Bureau.
Jesús Rivera-Román indicated no relevant financial relationships.
Karelys Burgos-Irizarry, MD1, Yue-Sai Jao-Ayala, MD1, Paola Laracuente-Román, MD2, José Muñoz-Acaba, MD3, Loscar Santiago-Rivera, MD3, Joham Senior-Marino, MD2, Jesús Rivera-Román, BS4. P0632 - Intestinal Phlebectasias: An Underestimated Cause of Overt Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
