Sunday Poster Session
Category: GI Bleeding
P0635 - A Rare Case of Ischemic Colitis: Two Hit Phenomenon by Vaginal Estrogen Ring and Heterozygous Prothrombin G20210A Mutation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- RC
Ryan Choi, DO
Naval Medical Center
San Diego, CA
Presenting Author(s)
Ryan Choi, DO, Jonathan Cho, MD, PhD, Maunoo Lee, MD, Leybelis Padilla, MD
Naval Medical Center, San Diego, CA
Introduction: We present an unusual case of ischemic colitis in the setting of vaginal estrogen ring and heterozygous prothrombin G20210A mutation.
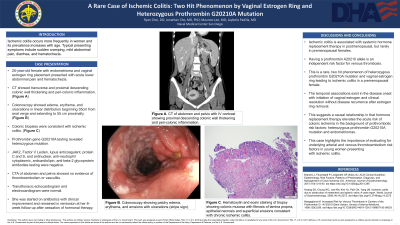
Case Description/Methods: A 25-year-old female with a history of endometriomas with recent vaginal estrogen ring placement presented with acute onset lower abdominal pain and hematochezia. Initial hemoglobin was 12.3 g/dL, ferritin was 12.11 ng/mL, and lactic acid was 0.9 mmol/L. Computed tomography of her abdomen and pelvis with intravenous contrast showed transverse and proximal descending colonic wall thickening without venous or arterial thromboembolism. Colonoscopy showed edema, erythema, and ulcerations in a linear distribution beginning 35cm from the anal verge and extending to 55cm proximally. Colonic biopsies returned concerning for ischemic colitis. Multiphase computed tomographic angiography of her abdomen and pelvis did not show thromboembolism or vasculitic changes. Prothrombin gene G20210A testing revealed heterozygous mutation. JAK2, Factor V Leiden, lupus anticoagulant, protein C and S, and antinuclear, antineutrophil cytoplasmic, anticardiolipin, anti-beta-2 glycoprotein antibodies testing were negative. Transthoracic echocardiogram and electrocardiogram were normal. She was started on Ciprofloxacin and Metronidazole for 7 days and her symptoms gradually improved. With cessation of systemic hormonal therapy, patient remained in remission without recurrence at her 8 week follow-up.
Discussion: Ischemic colitis is associated with systemic hormone replacement therapy in postmenopausal, but rarely in premenopausal females. We present a rare, two hit phenomenon of heterozygous prothrombin G20210A mutation and vaginal estrogen ring leading to ischemic colitis in a premenopausal female without other prothrombotic risk factors. The temporal associations between the initiation of vaginal estrogen ring with symptomatic onset and clinical resolution without recurrence after estrogen ring removal strongly favor a causal relationship that suggests hormone replacement therapy elevates the acute risk of colonic ischemia in the background of prothrombotic risk factors: heterozygous prothrombin G20210A mutation and endometriomas. This case highlights the importance of evaluating for underlying arterial and venous thromboembolism risk factors in young women presenting with ischemic colitis.

Disclosures:
Ryan Choi, DO, Jonathan Cho, MD, PhD, Maunoo Lee, MD, Leybelis Padilla, MD. P0635 - A Rare Case of Ischemic Colitis: Two Hit Phenomenon by Vaginal Estrogen Ring and Heterozygous Prothrombin G20210A Mutation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Naval Medical Center, San Diego, CA
Introduction: We present an unusual case of ischemic colitis in the setting of vaginal estrogen ring and heterozygous prothrombin G20210A mutation.
Case Description/Methods: A 25-year-old female with a history of endometriomas with recent vaginal estrogen ring placement presented with acute onset lower abdominal pain and hematochezia. Initial hemoglobin was 12.3 g/dL, ferritin was 12.11 ng/mL, and lactic acid was 0.9 mmol/L. Computed tomography of her abdomen and pelvis with intravenous contrast showed transverse and proximal descending colonic wall thickening without venous or arterial thromboembolism. Colonoscopy showed edema, erythema, and ulcerations in a linear distribution beginning 35cm from the anal verge and extending to 55cm proximally. Colonic biopsies returned concerning for ischemic colitis. Multiphase computed tomographic angiography of her abdomen and pelvis did not show thromboembolism or vasculitic changes. Prothrombin gene G20210A testing revealed heterozygous mutation. JAK2, Factor V Leiden, lupus anticoagulant, protein C and S, and antinuclear, antineutrophil cytoplasmic, anticardiolipin, anti-beta-2 glycoprotein antibodies testing were negative. Transthoracic echocardiogram and electrocardiogram were normal. She was started on Ciprofloxacin and Metronidazole for 7 days and her symptoms gradually improved. With cessation of systemic hormonal therapy, patient remained in remission without recurrence at her 8 week follow-up.
Discussion: Ischemic colitis is associated with systemic hormone replacement therapy in postmenopausal, but rarely in premenopausal females. We present a rare, two hit phenomenon of heterozygous prothrombin G20210A mutation and vaginal estrogen ring leading to ischemic colitis in a premenopausal female without other prothrombotic risk factors. The temporal associations between the initiation of vaginal estrogen ring with symptomatic onset and clinical resolution without recurrence after estrogen ring removal strongly favor a causal relationship that suggests hormone replacement therapy elevates the acute risk of colonic ischemia in the background of prothrombotic risk factors: heterozygous prothrombin G20210A mutation and endometriomas. This case highlights the importance of evaluating for underlying arterial and venous thromboembolism risk factors in young women presenting with ischemic colitis.

Figure: Ischemic colitis associated with vaginal estrogen ring and heterozygous prothrombin G20210A mutation. A. Computed tomography of abdomen and pelvis with intravenous contrast showing transverse and proximal descending colonic wall thickening and peri-colonic inflammation. B. Colonoscopy showing patchy edema, erythema, and erosions with ulcerations (stripe sign). C. Hematoxylin and eosin staining of biopsy tissue showing colonic mucosa with fibrosis of lamina propria, epithelial necrosis and superficial erosions consistent with chronic ischemic colitis.
Disclosures:
Ryan Choi indicated no relevant financial relationships.
Jonathan Cho indicated no relevant financial relationships.
Maunoo Lee indicated no relevant financial relationships.
Leybelis Padilla indicated no relevant financial relationships.
Ryan Choi, DO, Jonathan Cho, MD, PhD, Maunoo Lee, MD, Leybelis Padilla, MD. P0635 - A Rare Case of Ischemic Colitis: Two Hit Phenomenon by Vaginal Estrogen Ring and Heterozygous Prothrombin G20210A Mutation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
