Sunday Poster Session
Category: GI Bleeding
P0645 - Dieulafoy's Lesion of Esophagus: A Common Cause of GI Bleeding in an Uncommon Location
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Charles Yang, DO
Thomas Jefferson University
Voorhees, NJ
Presenting Author(s)
Charles Yang, DO1, Trinava Roy, DO1, Anjeli Patel, DO2, Joshua Soliman, DO1, Christopher Chhoun, DO1, Christopher Morrison, MD3
1Thomas Jefferson University, Voorhees, NJ; 2Einstein Medical Center, Philadelphia, PA; 3Virtua Health, Camden, NJ
Introduction: Dieulafoy’s lesions (DL) are established causes of gastrointestinal (GI) bleeding that are most commonly found in the lesser curvature of the stomach. There is a paucity of literature describing DLs in the esophagus. We present a case of an esophageal DL in a 61-year-old cirrhotic female.
Case Description/Methods: A 61-year-old female with a past medical history of alcoholic cirrhosis was admitted for hematemesis. Hemoglobin on admission was 10.6 g/dL. Initial esophagogastroduodenoscopy(EGD) demonstrated grade D esophagitis, mild gastritis and absence of varices with fresh blood without a definite source. At this point, she was accepted as a liver transplant candidate and upgraded to the intensive care unit for acute decompensated liver cirrhosis with hepatic encephalopathy. Unfortunately, on hospital day 16, the patient had a subsequent episode of bright red emesis and underwent a second EGD demonstrating similar esophagitis and gastritis. Hemoglobin was stable. On hospital day 34, the patient became acutely encephalopathic and hypotensive requiring vasopressors. Hemoglobin in the morning was 7.3 g/dL and repeat that afternoon was 5.9 g/dL. She underwent emergent intubation followed by repeat EGD demonstrating a small vessel with pulsatile bleeding consistent with a DL in the lower third of the esophagus which was managed with epinephrine, cauterization, and finally hemospray. Importantly, there was no esophageal or gastric ulcer noted. The patient could not overcome her acute hypoxic respiratory failure despite maximum ventilator support and ultimately expired.
Discussion: Esophageal DLs have been documented without defined incidence or prevalence. DLs in general account for 0.5%-14% of patients who develop acute upper GI bleeding. This vascular anomaly is an especially large caliber artery in the GI tract that has a propensity for catastrophic hemorrhage. DLs are most commonly found in the stomach within six centimeters of the gastroesophageal junction. Pathophysiology continues to be debated, but associations with chronic kidney disease, antiplatelet agents and hypertension have been made. Diagnosis relies primarily on endoscopic visualization. Other means of diagnosis such as endoscopic ultrasound and bleeding provocation have been utilized. The mainstay of treatment involves endoscopic injection, cautery and ligation. A scarcity of information exists regarding esophageal versus gastric DLs. This case highlights the course of a patient with Dieulafoy’s lesion in a notably uncommon location.

Disclosures:
Charles Yang, DO1, Trinava Roy, DO1, Anjeli Patel, DO2, Joshua Soliman, DO1, Christopher Chhoun, DO1, Christopher Morrison, MD3. P0645 - Dieulafoy's Lesion of Esophagus: A Common Cause of GI Bleeding in an Uncommon Location, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Thomas Jefferson University, Voorhees, NJ; 2Einstein Medical Center, Philadelphia, PA; 3Virtua Health, Camden, NJ
Introduction: Dieulafoy’s lesions (DL) are established causes of gastrointestinal (GI) bleeding that are most commonly found in the lesser curvature of the stomach. There is a paucity of literature describing DLs in the esophagus. We present a case of an esophageal DL in a 61-year-old cirrhotic female.
Case Description/Methods: A 61-year-old female with a past medical history of alcoholic cirrhosis was admitted for hematemesis. Hemoglobin on admission was 10.6 g/dL. Initial esophagogastroduodenoscopy(EGD) demonstrated grade D esophagitis, mild gastritis and absence of varices with fresh blood without a definite source. At this point, she was accepted as a liver transplant candidate and upgraded to the intensive care unit for acute decompensated liver cirrhosis with hepatic encephalopathy. Unfortunately, on hospital day 16, the patient had a subsequent episode of bright red emesis and underwent a second EGD demonstrating similar esophagitis and gastritis. Hemoglobin was stable. On hospital day 34, the patient became acutely encephalopathic and hypotensive requiring vasopressors. Hemoglobin in the morning was 7.3 g/dL and repeat that afternoon was 5.9 g/dL. She underwent emergent intubation followed by repeat EGD demonstrating a small vessel with pulsatile bleeding consistent with a DL in the lower third of the esophagus which was managed with epinephrine, cauterization, and finally hemospray. Importantly, there was no esophageal or gastric ulcer noted. The patient could not overcome her acute hypoxic respiratory failure despite maximum ventilator support and ultimately expired.
Discussion: Esophageal DLs have been documented without defined incidence or prevalence. DLs in general account for 0.5%-14% of patients who develop acute upper GI bleeding. This vascular anomaly is an especially large caliber artery in the GI tract that has a propensity for catastrophic hemorrhage. DLs are most commonly found in the stomach within six centimeters of the gastroesophageal junction. Pathophysiology continues to be debated, but associations with chronic kidney disease, antiplatelet agents and hypertension have been made. Diagnosis relies primarily on endoscopic visualization. Other means of diagnosis such as endoscopic ultrasound and bleeding provocation have been utilized. The mainstay of treatment involves endoscopic injection, cautery and ligation. A scarcity of information exists regarding esophageal versus gastric DLs. This case highlights the course of a patient with Dieulafoy’s lesion in a notably uncommon location.

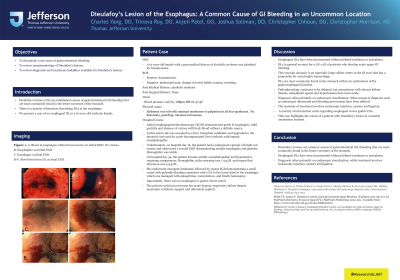
Figure: A. Blood in esophagus without focal source on initial EGD. No varices.
B. Esophagitis on initial EGD.
C. Esophagus on final EGD.
D-F. Slow bleed from DL on final EGD.
B. Esophagitis on initial EGD.
C. Esophagus on final EGD.
D-F. Slow bleed from DL on final EGD.
Disclosures:
Charles Yang indicated no relevant financial relationships.
Trinava Roy indicated no relevant financial relationships.
Anjeli Patel indicated no relevant financial relationships.
Joshua Soliman indicated no relevant financial relationships.
Christopher Chhoun indicated no relevant financial relationships.
Christopher Morrison indicated no relevant financial relationships.
Charles Yang, DO1, Trinava Roy, DO1, Anjeli Patel, DO2, Joshua Soliman, DO1, Christopher Chhoun, DO1, Christopher Morrison, MD3. P0645 - Dieulafoy's Lesion of Esophagus: A Common Cause of GI Bleeding in an Uncommon Location, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
