Sunday Poster Session
Category: GI Bleeding
P0647 - A Gut-Wrenching Case of Aortic Dissection Complicated by Acute Ischemic Duodenal Ulcer
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Shriraj Patel, DO
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Shriraj Patel, DO, Bing Chen, MD, Sunny Patel, DO
Geisinger Medical Center, Danville, PA
Introduction: Aortic dissection (AD) is a life-threatening condition characterized by degeneration of the aortic media, leading to the formation of a false lumen. The false lumen can expand and press on the true lumen, causing reduced blow flow and consequent ischemia to vital organs. Type B ADs can extend into the abdominal aorta, potentially narrowing its branches and compromising blood supply to the bowel. We present a rare case of a 65-year-old male with type B AD extending to the celiac trunk, resulting in an acute ischemic duodenal ulcer.
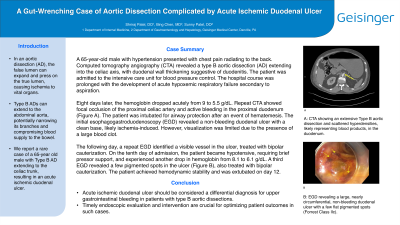
Case Description/Methods: A 65-year-old male with hypertension presented with chest pain radiating to the back. Computed tomography angiography (CTA) revealed a type B aortic dissection extending into the celiac axis, along with duodenal wall thickening suggestive of duodenitis. The patient was admitted to the intensive care unit for blood pressure control and developed acute respiratory failure following an aspiration event. Eight days later, the patient experienced an acute drop in hemoglobin from 9 to 5.5 g/dL. Repeat CTA showed focal occlusion of the proximal celiac artery and active bleeding in the proximal duodenum (Figure A). Hematemesis occurred, leading to intubation for airway protection. The initial esophagogastroduodenoscopy (EGD) revealed a large non-bleeding duodenal ulcer with a clean base, likely ischemia-induced. However, visualization of a significant portion of the duodenum was limited due to a large blood clot. The following day, a repeat EGD identified a visible vessel in the ulcer, treated with bipolar cauterization. On the tenth day of admission, the patient became hypotensive, requiring brief pressors, and experienced another drop in hemoglobin from 8.1 to 6.1 g/dL. A third EGD revealed a few pigmented spots in the ulcer (Figure B), also treated with bipolar cauterization. The patient achieved hemodynamic stability and was extubated on day 12.
Discussion: This case highlights a rare complication of type B aortic dissections, in which the extension of the false lumen into the celiac plexus can lead to acute ischemic duodenal ulcer. Acute ischemic duodenal ulcer should be considered a differential diagnosis for upper gastrointestinal bleeding in patients with type B aortic dissections. Timely endoscopic evaluation and intervention are crucial for optimizing patient outcomes in such cases.

Disclosures:
Shriraj Patel, DO, Bing Chen, MD, Sunny Patel, DO. P0647 - A Gut-Wrenching Case of Aortic Dissection Complicated by Acute Ischemic Duodenal Ulcer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Geisinger Medical Center, Danville, PA
Introduction: Aortic dissection (AD) is a life-threatening condition characterized by degeneration of the aortic media, leading to the formation of a false lumen. The false lumen can expand and press on the true lumen, causing reduced blow flow and consequent ischemia to vital organs. Type B ADs can extend into the abdominal aorta, potentially narrowing its branches and compromising blood supply to the bowel. We present a rare case of a 65-year-old male with type B AD extending to the celiac trunk, resulting in an acute ischemic duodenal ulcer.
Case Description/Methods: A 65-year-old male with hypertension presented with chest pain radiating to the back. Computed tomography angiography (CTA) revealed a type B aortic dissection extending into the celiac axis, along with duodenal wall thickening suggestive of duodenitis. The patient was admitted to the intensive care unit for blood pressure control and developed acute respiratory failure following an aspiration event. Eight days later, the patient experienced an acute drop in hemoglobin from 9 to 5.5 g/dL. Repeat CTA showed focal occlusion of the proximal celiac artery and active bleeding in the proximal duodenum (Figure A). Hematemesis occurred, leading to intubation for airway protection. The initial esophagogastroduodenoscopy (EGD) revealed a large non-bleeding duodenal ulcer with a clean base, likely ischemia-induced. However, visualization of a significant portion of the duodenum was limited due to a large blood clot. The following day, a repeat EGD identified a visible vessel in the ulcer, treated with bipolar cauterization. On the tenth day of admission, the patient became hypotensive, requiring brief pressors, and experienced another drop in hemoglobin from 8.1 to 6.1 g/dL. A third EGD revealed a few pigmented spots in the ulcer (Figure B), also treated with bipolar cauterization. The patient achieved hemodynamic stability and was extubated on day 12.
Discussion: This case highlights a rare complication of type B aortic dissections, in which the extension of the false lumen into the celiac plexus can lead to acute ischemic duodenal ulcer. Acute ischemic duodenal ulcer should be considered a differential diagnosis for upper gastrointestinal bleeding in patients with type B aortic dissections. Timely endoscopic evaluation and intervention are crucial for optimizing patient outcomes in such cases.

Figure: Figure 1. Radiographic and Endoscopic Findings:
A. Cross-sectional view on computed tomography angiography (CTA) showing an extensive Type B aortic dissection and scattered hyperdensities, likely representing blood products, in the duodenum.
B. Esophagogastroduodenoscopy (EGD) image revealing a large, nearly circumferential, non-bleeding duodenal ulcer with a few flat pigmented spots (Forrest Class IIc)
A. Cross-sectional view on computed tomography angiography (CTA) showing an extensive Type B aortic dissection and scattered hyperdensities, likely representing blood products, in the duodenum.
B. Esophagogastroduodenoscopy (EGD) image revealing a large, nearly circumferential, non-bleeding duodenal ulcer with a few flat pigmented spots (Forrest Class IIc)
Disclosures:
Shriraj Patel indicated no relevant financial relationships.
Bing Chen indicated no relevant financial relationships.
Sunny Patel indicated no relevant financial relationships.
Shriraj Patel, DO, Bing Chen, MD, Sunny Patel, DO. P0647 - A Gut-Wrenching Case of Aortic Dissection Complicated by Acute Ischemic Duodenal Ulcer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
